A common culprit drives prostate cancer progression
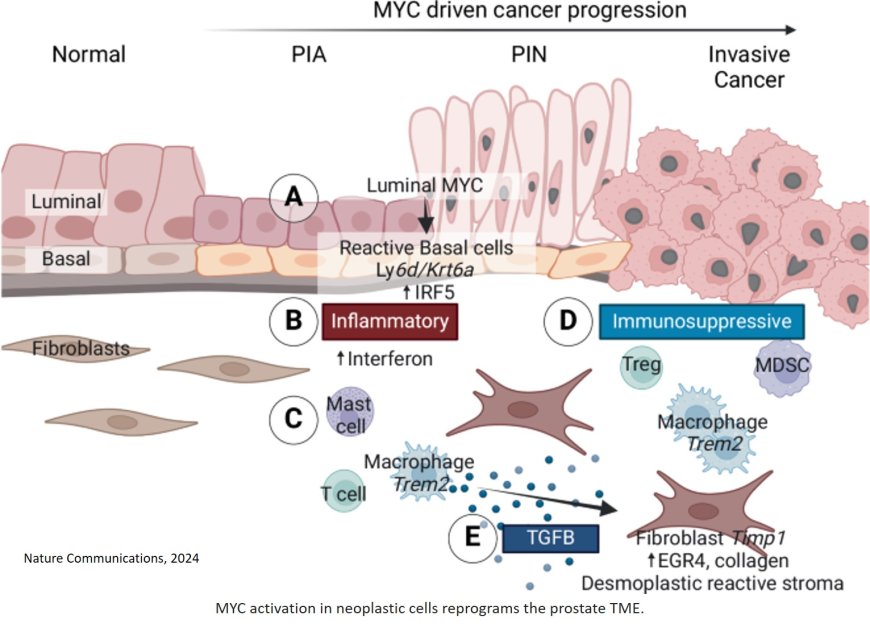
By tracking the changes in prostate cancer cells over time, researchers have found that activation of the MYC gene — a well-known cancer-causing gene — sets off a cascade of events that leads to both initiation and progression of the disease.
Scientists have learned that prostate cancers can vary significantly among patients and that there are often differences within each patient’s tumor. However, the study published in Nature Communications identifies the MYC gene as a common denominator across prostate cancers. The work demonstrates that initial MYC activation attracts immune cells to the tumor but later helps hide the tumor from immune cells. This discovery is the first step toward identifying potential therapeutic targets along the pathway.
“This is a very powerful oncogenic pathway set off by MYC activation,” says the senior author. “We need to understand this complex cascade of events in detail to find out more effective ways to manage the disease.”
Studies of human tumor tissues can help scientists investigate prostate cancer, but they only provide a snapshot. To get a sense of the changes that occur over time in prostate cancer, scientists turn to animal models. The researchers married the two approaches to get a detailed look at prostate cancer initiation and progression.
The team used single-cell RNA sequencing to show that targets of the MYC gene are overexpressed in human tumor tissue samples, indicating increased MYC activity. Then, they watched what unfolds in animal models of prostate cancer after MYC activity ramps up.
The researchers found that when MYC initially becomes upregulated in precancerous cells, activity increases in pathways that alert the immune system that something is wrong. But eventually, the immune-attracting pathways are turned off. As the tumor progresses, it stops signaling to the immune system and goes undetected. The discovery may help explain why prostate cancers don’t respond well to immunotherapies that act by removing the brakes on the immune system’s response to cancer — if the immune system is not working to begin with, lifting those brakes will not help.
“These prostate cancer cells have learned how to turn off the signals that would otherwise alert the immune system, allowing them to evade the immune system,” the author says. “Now, we can try to develop strategies to re-engage the immune response and sensitize the tumors to immunotherapy.”
Drugs targeting TREM2 macrophages — some of the immune cells affected by excess MYC expression in prostate cancer — are already in development and are potential tools to help the immune system fight prostate tumors.
The study, which also used molecular pathology techniques, showed that increased MYC expression and activity starts in epithelial cells lining the prostate. Eventually, the epithelial cells become cancer cells, which signal to surrounding cells, dampening the immune response, causing scarring, expanding the number of tumor cells, and inducing other molecular changes. The study results strengthen the evidence that MYC may be a critical target for prostate cancer treatment or prevention, the author says.
“We’ve seen some of these changes in human prostate tumors for a long time, but we didn’t understand that the whole process could be set off by one inciting event: upregulation of MYC,” the author says.