Common brain network detected among veterans with PTSD
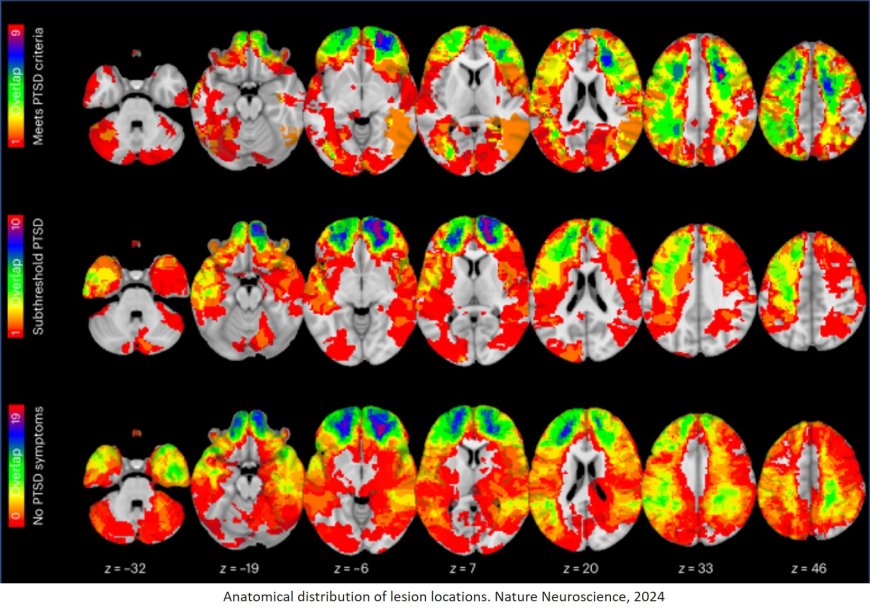
A new study suggests that using neurostimulation therapies on a specific brain network could treat post traumatic stress disorder (PTSD) in veterans. By evaluating 193 participants with penetrating traumatic brain injury, the team found those with damage connected to their amygdala, the fear center of the brain, were less likely to develop PTSD. Their results are published in Nature Neuroscience.
“This is a very real brain disease, and we can localize it to certain brain circuits,” said the corresponding author. “Unfortunately, people sometimes assume PTSD has to do with how mentally strong or weak a person is, but it has nothing to do with moral character.”
“The amygdala is deep in the brain, making it hard to hit precisely with a stimulation modality without doing surgery,” the author said.
The team examined 193 patients with penetrating traumatic brain injuries from the Vietnam Head Injury. They looked at whether those veterans developed PTSD 20 years after the war in Vietnam.
“Some of these veterans who got shrapnel in their head went on to develop PTSD, but many of them did not,” the author said. “The patients actually developed PTSD less than other veterans who did not get damage to their brain.”
Researchers then hypothesized that a circuit must exist that, when damaged, protects against PTSD. They used their wiring diagram, the human connectome, to map where brain damage had occurred and where each lesion connected. From there, they compared the data to 180 veterans who did not have brain damage, some of whom have PTSD and some whom do not. They found connectivity within the circuit correlated with whether they had PTSD or not. Finally, the team looked at whether this circuit would be a good target for treatment by examining previous trials using TMS for PTSD.
“The trials where stimulation was hitting the circuit we identified tended to be the trials that had good outcomes in patients,” the author said. “We also asked whether or not our results could inform how to stimulate the targets, leading to what we believe is a therapeutic target for treatment using TMS.”
During the study, a patient with severe PTSD requested TMS. After a careful informed consent process, clinicians used the circuit found in the study to treat the patient, ultimately improving his symptoms.
The author said while it’s only one patient, the case provides an illustration for how the results of the study might translate into a clinical setting. Before it can be accessible to a larger population, they will have to conduct a randomized controlled trial targeting the circuit to gain FDA approval.
The senior author said one limitation to the study is they don’t yet know how the treatment results could change if a person is in a state of PTSD-induced fear at the time of treatment compared to relaxation. The other author added the study included only veterans, so they are unsure if PTSD in non-veterans would map onto the same circuit.
“While more work remains to be done, we’ve taken an important step here to identify a therapeutic target for a condition in patients who desperately need better treatments,” the author said.
https://www.nature.com/articles/s41593-024-01772-7