Common food poison toxin speeds colon cancer spread
A toxin in the bacteria that’s one of the most common causes of foodborne illness accelerates the spread of colorectal tumors to other parts of the body, a study has found.
The findings, published in the journal Cell Host & Microbe, could pave the way for new tools to detect metastatic colorectal cancer early and could ultimately help determine patients who need more aggressive treatments.
“This work contributes to a new understanding of how bacterial toxins promote colorectal metastasis, opening novel screening approaches to predict at-risk patients,” said the lead author.
The intestinal microbiota is the collection of microorganisms that live in the gut. These microorganisms are known to play a wide-ranging role in health, from digestion to regulation of the immune system. They also influence the development and spread of several types of cancer, including colorectal.
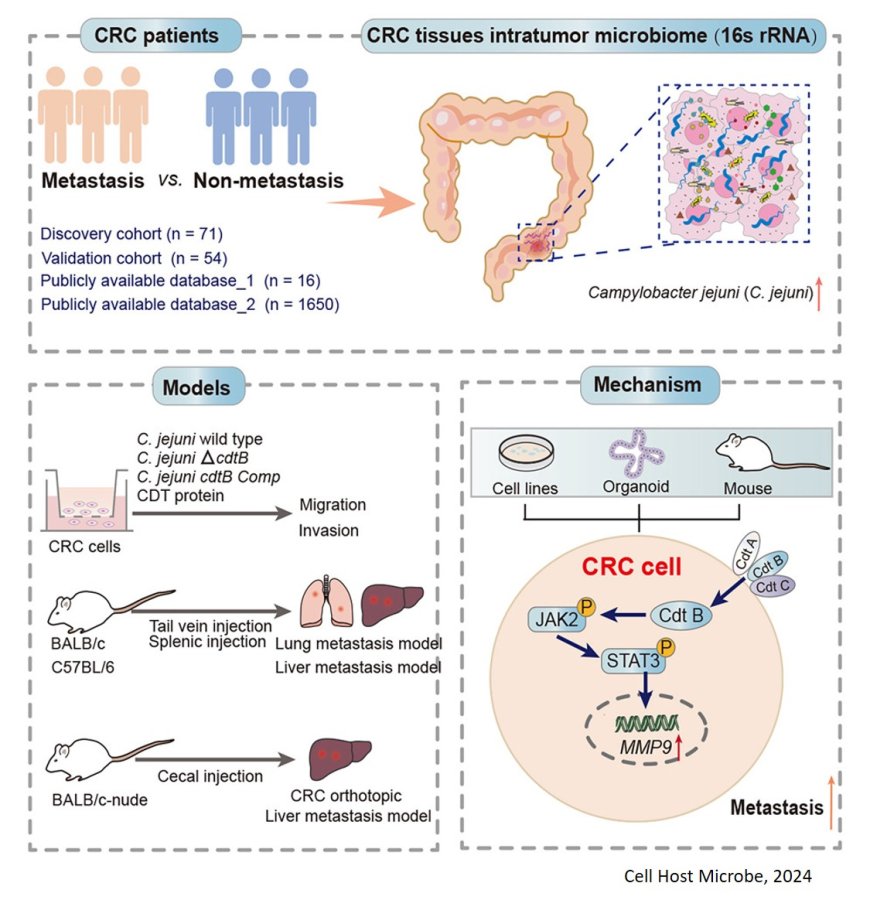
Campylobacter jejuni (C. jejuni) is a bacterium that causes more than 2 million cases of diarrheal-related illness each year in the United States. Some C. jejuni species have a toxin called cytolethal distending toxin, or CDT. Previously researchers showed that this toxin was essential to causing colorectal cancer in mice.
In the new study, the team set out to find how the bacteria affect the spread of cancer. Colorectal cancer is the second-leading cause of cancer death in the United States, but when it’s caught early, before it has spread, the five-year relative survival rate is about 90%. Metastases, or secondary growths formed away from the initial cancer site, are the primary cause of death from cancer, and treatment options for these patients remain limited.
The team first compared the presence of C. jejuni in tissues from 34 patients with primary colorectal cancer who ended up developing metastasis with 37 patients who did not develop metastasis within a three-year follow-up period.
They found a significant presence of the bacteria in the patients with metastasis. Notably, patients with detectable levels of the bacteria had a significantly poorer outlook than those without. The team confirmed these findings in large national data sets of tumor samples.
“These findings confirmed that CDT is essential for the bacteria’s role in promoting cancer spread,” the author said. “When bacteria that produce CDT move to tumors outside the gut, it appears to accelerate the spread of these tumors.”
Using laboratory mice with metastatic lung and liver tumors, human colorectal cancer tissue, and 3D colorectal cancer tumor models made from patient cells, the researchers showed how the bacterial toxin promoted the spread of cancer. They found CDT led to an increased expression of several types of enzymes and activated a type of signaling in cancer cells associated with metastasis.
Several clinical trials are testing drugs that aim to interfere with that cell-signaling pathway, meaning the findings may guide the development of new therapies, the researchers said.
The researchers also recovered live bacteria from tumors outside the gut, suggesting the tumors created an environment that was friendly to their growth. More research is needed to understand how the bacteria migrated to tumor sites and how the toxin activates the signaling pathways.
https://www.cell.com/cell-host-microbe/fulltext/S1931-3128(24)00437-2