Dysfunctional mitochondria disrupt the gut microbiome in Crohn’s disease
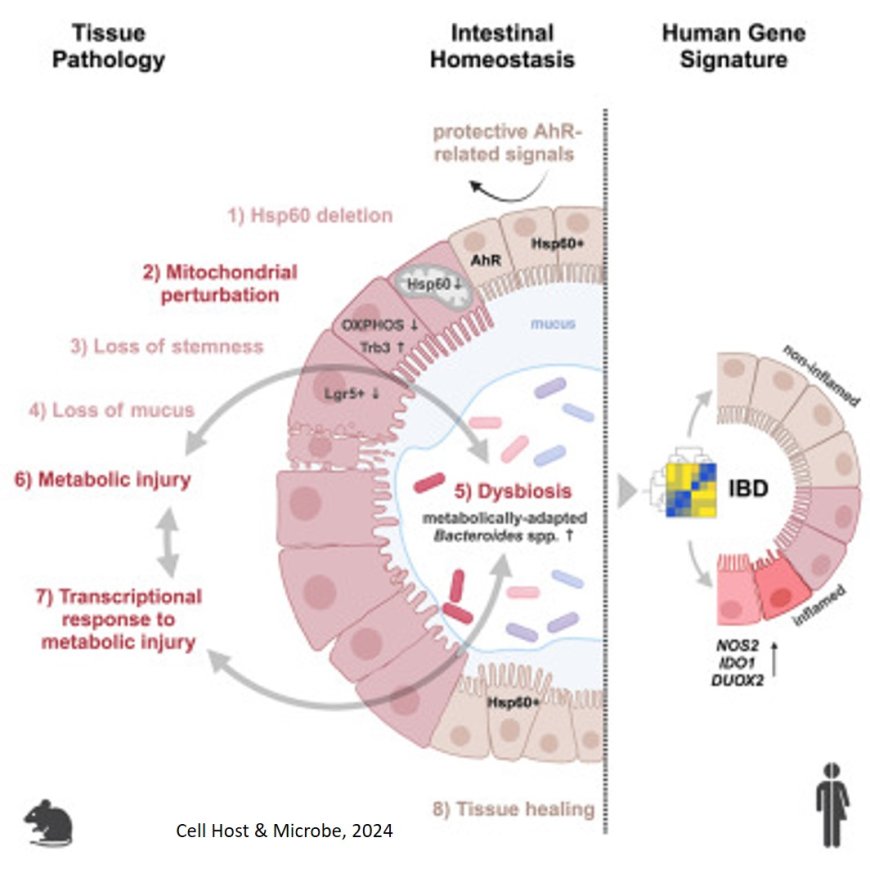
Typical symptoms of Crohn’s disease (CD) include chronic diarrhea, abdominal pain and fever. Although the causes of Crohn’s disease are not yet fully understood, it has been known for some years that changes in the gut microbiome (that is to say the community of microbes that live in the intestinal tract) are associated with inflammatory diseases. Some researchers see these changes – the causes of which remain unknown – as the trigger of the disease.
A team of researchers have searched for the causes of this changes in the microbiome and investigated the interplay of the microbiome, the intestinal epithelium and mitochondria. The intestinal epithelium is a cell layer that lines the inside of the intestine, absorbs nutrients and fights off pathogens. Mitochondria are small cellular structures that convert nutrients into energy and therefore influence the cellular metabolism and the ability of cells to perform their functions.
The team has been pursuing the hypothesis that mitochondria not only serve as the power plants of cells, but also interact with the microbiome. In addition, previous research has shown that the intestinal epithelium in patients with chronic intestinal inflammation exhibit certain stress markers indicating possible mitochondrial malfunction.
For their study the researchers therefore disrupted mitochondrial function in mice by deleting a gene segment responsible for producing the protein Hsp60. This protein is essential to the ability of mitochondria to perform their tasks. The intervention triggered various processes in the gut. For one, tissue injuries were identified in the intestinal epithelium similar to those seen in Crohn’s disease patients. Changes were also seen at the level of gene activation that are typical of some stages of the disease. In addition – an essential development for the question investigated by the team – the microbiome responded to the disrupted mitochondria by changing its composition.
As a result, the team were able to demonstrate for the first time that disruptions to mitochondria are causally related to tissue damage in the intestines and also trigger disease-related changes in the microbiome.
This insight may prove important to persons with inflammatory conditions because it presents potential approaches for new treatments. Currently, treatment is limited to alleviating the symptoms of the disease with anti-inflammatory medications.
“The big hope is to find active ingredients that would restore the functionality of disrupted mitochondria, in other words to repair them in a sense. This would limit intestinal damage as a trigger for chronic inflammation processes”, says the author. “Our results suggest that drugs that act on mitochondrial pathways or address the connections between the microbiome and mitochondria could be a key aspect of better treatments.”
https://www.cell.com/cell-host-microbe/fulltext/S1931-3128(24)00231-2