Key protein in the inflammatory pathway driving fatty liver disease
Scientists have dissected the key signalling mechanism driving inflammation in metabolic dysfunction-associated steatohepatitis (MASH), through which they have also uncovered a promising new protein target to combat the fatty liver disease.
With a 5.9% prevalence in Singapore that is projected to grow to 7.5% in 2030 [1], MASH is a chronic and progressive type of fatty liver disease in which fat build-up in the liver triggers immune cells to accumulate and react, causing inflammation. Further implicated by other rising metabolic disorders (such as obesity and type 2 diabetes) as risk factors, it is one of the leading causes of liver-related morbidity and mortality, with no approved treatments currently available to halt its progression.
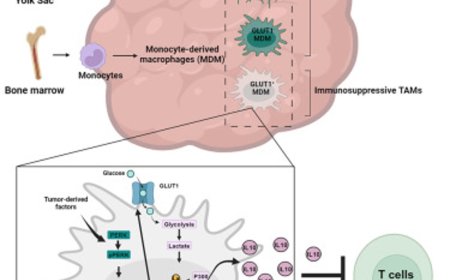
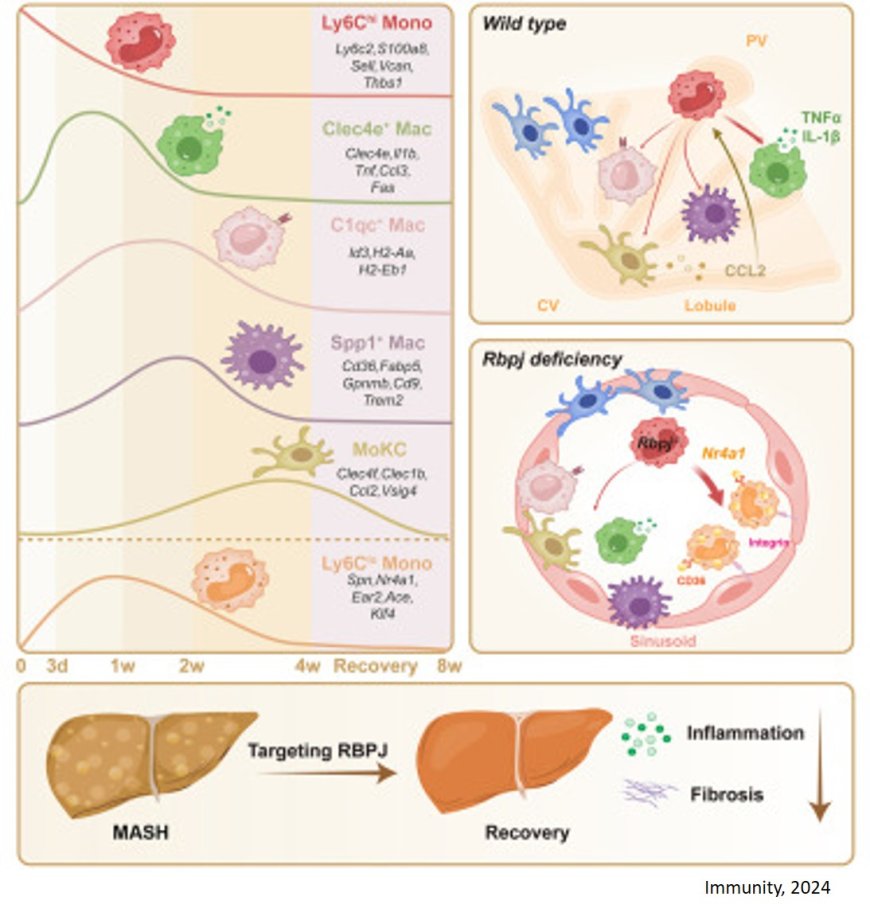
In their paper published in Immunity, the research team used advanced single-cell RNA sequencing, lineage tracing and mouse models to identify that the Notch signalling pathway controls the conversion of monocytes into inflammatory macrophages, a process critical to MASH development. Taking control of this pathway through the Recombination signal binding protein for immunoglobulin kappa J region (Rbpj) protein, the scientists were able to reroute the production of these inflammatory macrophages to protective monocytes instead.
The liver has its own native population of immune cells that stick to the endothelial cells surrounding the liver capillaries. Together, they act as the gatekeepers of immunity, filtering or scavenging harmful microorganisms, dead debris and lipids (fats) from incoming blood. However, when there are too many lipids, the environment turns toxic, killing the native immune cells and stressing the endothelial cells to trigger inflammatory response. The scientists found how this summons non-native monocytes to the liver, and how Notch signalling transforms them into inflammatory macrophages.
Probing deeper, the scientists discovered as well that removing Rbpj, a seminal protein in the Notch pathway, not only blocks those non-native monocytes from turning into inflammatory macrophages, but also allows them to transform into protective monocytes instead. These protective monocytes possess more lipid-scavenging receptors and can take up more lipids, thereby helping to protect the endothelial cells and quell inflammation.
This distinctive, dual function of Rbpj makes it a key therapeutic target in inventing new reparative strategies for MASH. Applying a simple treatment of nanoparticles carrying Rbpj inhibitors was able to successfully retard inflammation and lower the grade of the MASH, proving to be an extremely effective and targeted solution with no side-effects.
“The Notch signalling pathway, and the immune cells involved, is not only well-conserved across species, but also across organs and inflammatory diseases,” said the author. “With this knowledge, we are interested in applying this study and treatment to other tissues and diseases with inflammatory pathways as the next step of our research.”
This highly-conserved nature of the Notch signalling pathway also presents an optimistic outlook for clinical testing, as there is a good chance that successful treatments in mice can be efficaciously applied to human patients.
Current treatments are primarily focused on metabolic mediation, but by targeting Rbpj in the Notch signalling pathway, there is hope that a new class of therapies directly addressing the underlying drivers of MASH could be made available.
https://www.cell.com/immunity/abstract/S1074-7613(24)00414-X