Mechanisms of anti-NMDAR autoimmune encephalitis
Imagine you wake up in a hospital without a single memory of the last month. Doctors say you had a series of violent episodes and paranoid delusions. You’d become convinced you were suffering from bipolar disorder. Then, after a special test, a neurologist diagnoses you with a rare autoimmune disease called anti-NMDAR encephalitis. This is what happened to Susannah Cahalan, a New York Post reporter who would go on to write the best-selling memoir Brain on Fire: My Month of Madness.
Anti-NMDAR encephalitis can lead to hallucinations, blackouts, and psychosis, says the senior author. It mostly affects women ages 25 to 35—the same age at which schizophrenia often presents itself. But what’s happening in anti-NMDAR encephalitis is something else.
“In anti-NMDAR encephalitis, antibodies bind to those receptors and prevent them from working,” the author explains. As an autoimmune response, the brain becomes inflamed—hence, Brain on Fire.
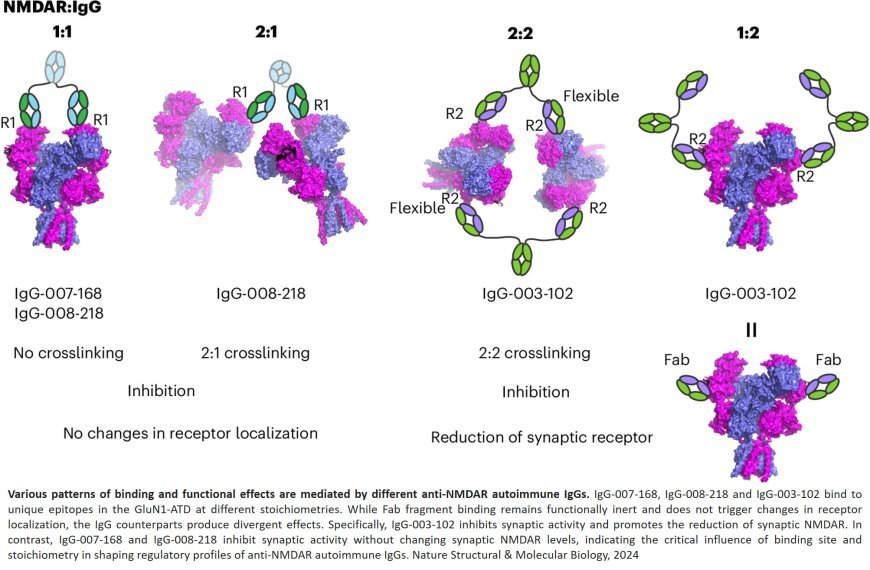
While some treatments are available, their effectiveness varies depending on symptom severity. New research from the lab may explain why. In a recent study, the authors determined structures of human and rat NMDARs bound to three distinct patient-derived antibodies using single-particle electron cryo-microscopy. These antibodies bind different regions within the amino-terminal domain of the GluN1 subunit.
All three autoantibodies acutely and directly reduced NMDAR channel functions in primary neurons. One antibody, also results in reduced synaptic localization of NMDARs.
“Distinct binding patterns manifest in different functional regulation levels in NMDARs,” the author explains. “This affects neuronal activities. So, different binding sites may correspond to variations in patients’ symptoms.” Uncovering those correlations could lead to more precise therapeutic strategies. Imagine, for example, that scientists identify several binding sites common among encephalitis patients. Pharmacologists could then design new drugs to target these sites. But that’s not all. Personalized medicine could also mean more accurate diagnoses, the author says.
“It’s still a rare disease, but it could be misdiagnosed or underdiagnosed. Therefore, we need to spread awareness. Could, for example, some schizophrenic patients have this disease? Could it be caused by antibodies?”