Special immune cells stop metastatic cancer

Metastatic disease—when cancer spreads from the primary tumor to other parts of the body—is the cause of most cancer deaths. While researchers understand how cancer cells escape the primary site to seed new tumors, it’s not well understood why some of these wayward cancer cells spawn new tumors— sometimes decades later—while others do not.
Now, a research team has discovered a natural immune mechanism in mice that stops escaped cancer cells from developing into tumors elsewhere in the body. The findings were published in the journal Cell.
“Preventing or curing metastases is the most critical challenge in cancer,” said study leader. “We think our findings have the potential to point to new therapies to prevent or treat metastatic disease.”
Cells that migrate from primary tumors and seed metastatic tumors are called disseminated cancer cells (DCCs). Some DCCs behave aggressively, immediately starting tumors in new tissue, while others remain in a state of suspended animation referred to as dormancy.
“It’s long been a mystery how some DCCs can remain in tissues for decades and never cause metastases, and we believe we’ve found the explanation,” said the lead author.
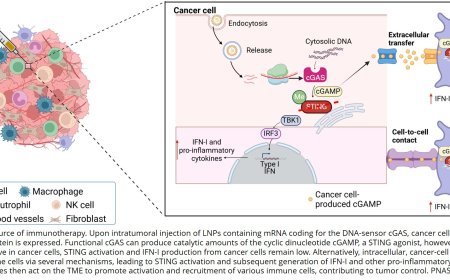
Breast cancer and many other types of cancer metastasize to the lungs. In research involving three mouse models of metastatic breast cancer, the researchers determined that when breast cancer DCCs spread to the lung’s air sacs (alveoli), they are kept in a dormant state by immune cells known as alveolar macrophages.
“Alveolar macrophages are the lung’s first responders, defending the organ against bacteria and dangerous substances like environmental pollutants,” said the author. These specialized macrophages, the author notes, appear early in embryonic development and reside within lung tissue for life.
“Our findings demonstrate a new role for these macrophages, in which they recognize DCCs and actively interact with them, and—by secreting a protein called TGF-β2—produce signals in the cancer cells that keep them in a dormant state,” the author said. “Since every organ in the body has its own set of tissue-resident macrophages, they may function to keep DCCs in check in those organs as well. Our study has shown for the first time that these specialized macrophages function to actively induce dormancy in DCCs.”
Confirming the importance of alveolar macrophages in keeping DCCs dormant, the team found that depleting them in the mice significantly increased the number of activated DCCs and subsequent metastases in their lungs compared to mice with normal levels of the immune cells.
As DCCs become more aggressive, the researchers found, they become resistant to the pro-dormancy signals produced by alveolar macrophages. Ultimately, this evasion mechanism enables some DCCs to “wake up” from dormancy and reactivate to form metastases.
“Understanding how immune cells keep DCCs in check could lead to new anti-metastatic cell therapies among other strategies,” the author said. For example, the author noted, it may be possible to strengthen macrophage signaling so that DCCs never awaken from dormancy or find ways to prevent older DCCs from becoming resistant to dormancy signaling.