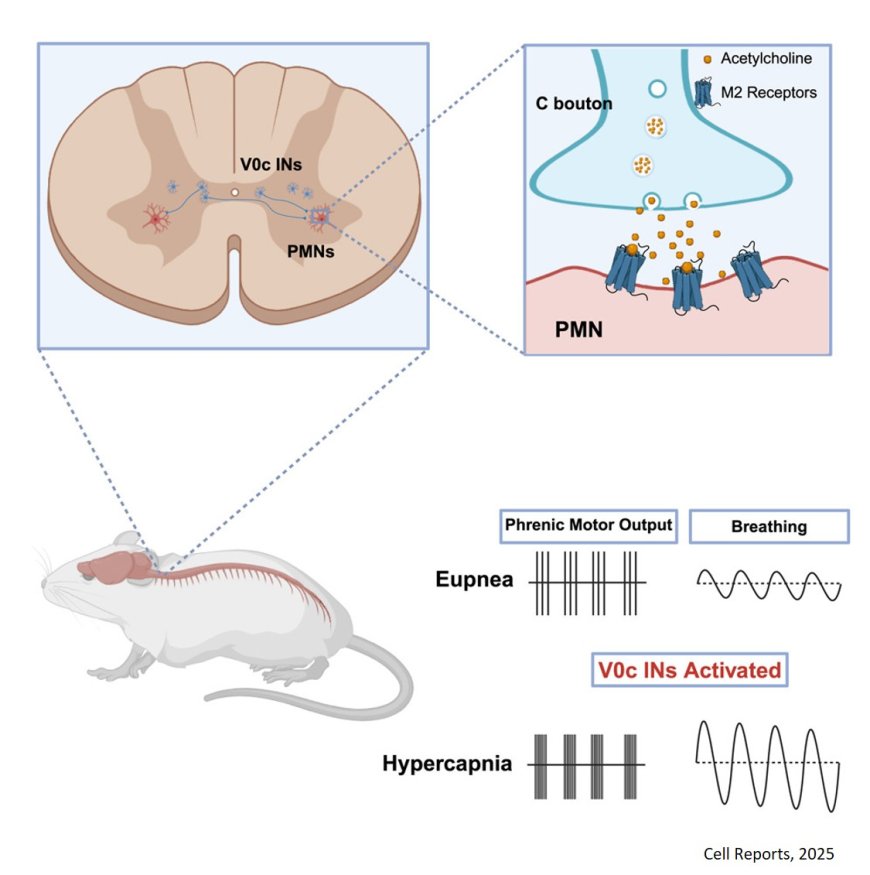
Breathing control by a cholinergic spinal pathway
Today about 300,000 people nationally living with a spinal cord injury and with respiratory complications being the most common cause of illness and death, according to the Christopher & Dana Reeve Foundation.
But the results of a new study show promise that a group of nerve cells in the brain and spinal cord—called interneurons—can boost breathing when the body faces certain physiological challenges, such as exercise and environmental conditions associated with altitude.
The researchers believe their discovery could lead to therapeutic treatments for patients with spinal cord injuries who struggle to breathe on their own. Their findings were recently published in the journal Cell Reports.
“While we know the brainstem sets the rhythm for breathing,” said the lead researcher, “the exact pathways that increase respiratory motor neuron output, have been unclear—until now.”
High-intensity motor neuron (MN) actions are critical for breathing that must be rapidly adjusted to accommodate changing metabolic demands
By identifying a subset of phrenic motor neurons (PMNs) as a new and potentially easy-to-reach point for treatment in spinal cord injuries and breathing-related diseases, the researchers believe doctors may be able to develop therapies to help improve breathing in people with such conditions.
The study showed that blocking signals from these spinal cord cells made it harder for the body to breathe properly when there was too much carbon dioxide (CO2) in the blood, a condition known as hypercapnia.
CO2 is created in the body when cells make energy. Red blood cells carry CO2 from organs and tissues to the lungs, where it is exhaled. If the body can’t shed CO2, it can build up in the blood, making it hard to breathe and leading to respiratory failure.
“These spinal cord cells are important for helping the body adjust its breathing in response to changes like high CO2 levels,” the author said.
In this study, the team used genetically modified mouse models to explore the pathways involved in breathing. The researchers mapped neuron connections, measured neuron electrical activity, observed the models’ behavior and used microscopy to visualize neuron structure and function—all focused on spinal cord nerve cells involved in breathing.
“We were able to define the genetic identity, activity patterns and role of a specialized subset of spinal cord neurons involved in controlling breathing,” the author said.
The team is now testing whether targeting these neurons in neurodegenerative diseases like amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease, and Alzheimer’s disease can help restore breathing.
https://www.cell.com/cell-reports/fulltext/S2211-1247(25)00849-6