Association between placental DNA methylation and schizophrenia
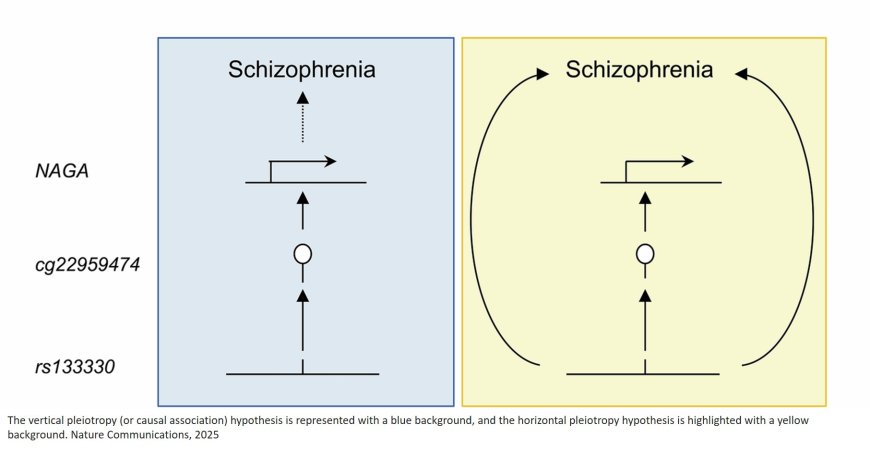
The study highlights the placenta as a key element in neuropsychiatric development. The research has demonstrated that specific epigenetic modifications in the placenta, particularly DNA methylation, can influence the expression of genes associated with psychiatric disorders. These findings suggest that genetic risk may already manifest during the prenatal stage.
Epigenetic modifications are chemical changes in DNA and its associated proteins that regulate gene activity without altering their sequence. One of the most studied modifications is DNA methylation, a process in which methyl groups—small molecules composed of one carbon and three hydrogen atoms—are added to specific regions of the DNA. This mechanism, essential for development, environmental adaptation, and disease predisposition, is influenced by genetics and responds to factors such as diet, stress, and exposure to pollutants.
The study results indicate that schizophrenia, bipolar disorder, and major depression disorder are the neuropsychiatric disorders most strongly linked to DNA methylation in the placenta. Other conditions, such as attention deficit hyperactivity disorder (ADHD) or autism, show some potentially causal associations, although to a lesser extent, while no visible effects were found in other analyzed pathologies.
“These findings reinforce the hypothesis that schizophrenia and other disorders have a neurodevelopmental origin and that the placenta plays a fundamental role in this process,” explains the author.
The discovery that genetic risk may be linked to placental DNA methylation opens new avenues for preventing and treating psychiatric disorders. “If we could identify risk factors at the prenatal stage, we could intervene before symptoms appear, adjusting treatments or designing personalized preventive strategies,” adds another author.
The study also underscores the importance of understanding where and when each genetic factor acts in pathology, since this could impact therapeutic decision-making. “Not all genes associated with a disorder should be treated directly; some may have acted in an earlier developmental stages and may not be actionable in adulthood,” concludes the author.
This research represents a significant advance in understanding the biological basis of neuropsychiatric disorders and opens new lines of investigation for early detection, as well as for the development of more effective therapies.
https://www.nature.com/articles/s41467-025-57760-3
https://sciencemission.com/placental-DNA-methylation-and-schizophrenia