Decoupling inflammation from pain
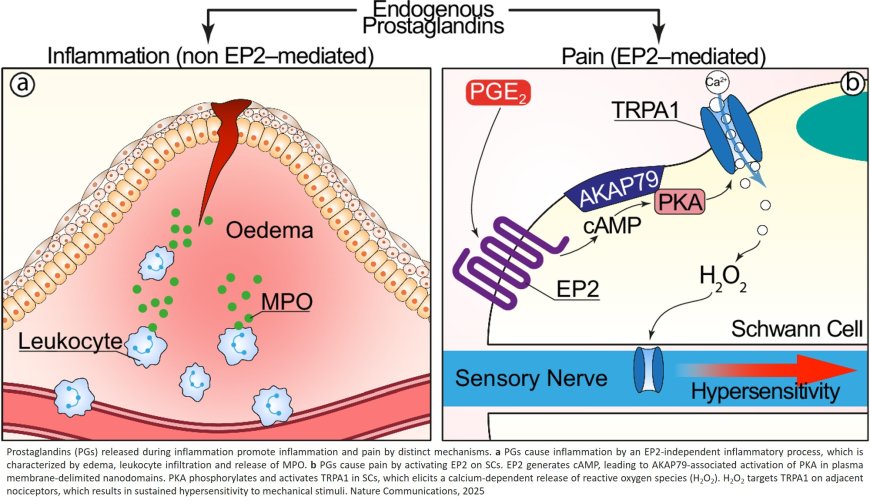
Scientists have identified which receptor in prostaglandins—the hormone-like substance targeted by common painkillers—causes pain but not inflammation. The findings, published in the journal Nature Communications, may help researchers to develop more selective drugs to treat pain with fewer side effects.
“Inflammation and pain are usually thought to go hand in hand. But being able to block pain and allow inflammation—which promotes healing—to proceed is an important step in improved treatment of pain,” said the senior study author.
Non-steroidal anti-inflammatory drugs, or NSAIDs, are among the most commonly taken medicines in the world, with an estimated 30 billion doses each year in the US alone. The drugs are available both over the counter (e.g., ibuprofen or aspirin) and as prescription medications. Unfortunately, long-term use of most NSAIDs carries serious risks, including damage to the lining of the stomach, increased bleeding, and issues with the heart, kidneys, and liver.
NSAIDs work by blocking enzymes that produce prostaglandins, reducing the level of prostaglandins, inflammation, and pain. Scientists commonly believe that getting rid of inflammation is what treats the pain. However, inflammation—the immune system's response to injury or infection—can be protective.
“Inflammation can be good for you—it repairs and restores normal function,” said study co-author. “Inhibiting inflammation with NSAIDs may delay healing and could delay recovery from pain. A better strategy to treat prostaglandin-mediated pain would be to selectively reduce the pain without affecting inflammation’s protective actions.”
In their study, the researchers focused on prostaglandin E2 (PGE2), which is considered a main mediator of inflammatory pain, in Schwann cells. Schwann cells are found outside the brain in the peripheral nervous system and play an important role in migraine and other forms of pain.
PGE2 has four different receptors. prior studies point to the EP4 receptor for PGE2 as the main receptor involved in producing inflammatory pain. However, in the Nature Communications study, the researchers used a more targeted approach and found that a different receptor—EP2—was largely responsible for pain. Delivering drugs locally to silence only the EP2 receptor in Schwann cells removed pain responses in mice without affecting inflammation.
“To our great surprise, blocking the EP2 receptor in Schwann cells abolished prostaglandin-mediated pain but the inflammation took its normal course. We effectively decoupled the inflammation from the pain,” said the author.
In additional studies in human and mouse Schwann cells, activating the EP2 receptor evoked a signal that sustained pain responses through a pathway independent from inflammatory responses, confirming the role of EP2 in pain but not inflammation.
“Antagonism of this ‘druggable’ receptor would thus control pain without the adverse effects of NSAIDs,” noted the author.
The researchers are continuing pre-clinical studies to explore how drugs that target the EP2 receptor could be used to treat pain in conditions like arthritis that would usually be treated with NSAIDs.
“Selective EP2 receptor antagonists could be very useful. While more research is needed on side effects, especially with giving a drug systemically as a pill, targeted administration that acts locally on an area like a knee joint holds promise," said the author.
https://www.nature.com/articles/s41467-025-63782-8
https://sciencemission.com/PGE2-receptor--in-Schwann-cells-inhibits-pain