Early ALS pathogenesis is driven by SMN complex dysregulation
Approximately 5,000 people in the U.S. develop amyotrophic lateral sclerosis (ALS) each year. On average, they survive for only two to five years after being diagnosed, according to the Centers for Disease Control and Prevention. The rapidly progressing neurodegenerative disease causes the death of neurons in the brain and spinal cord, resulting in muscle weakness, respiratory failure and dementia. Despite the devastating nature of the disease, little is known about what first triggers the deterioration of motor neurons at the onset of ALS.
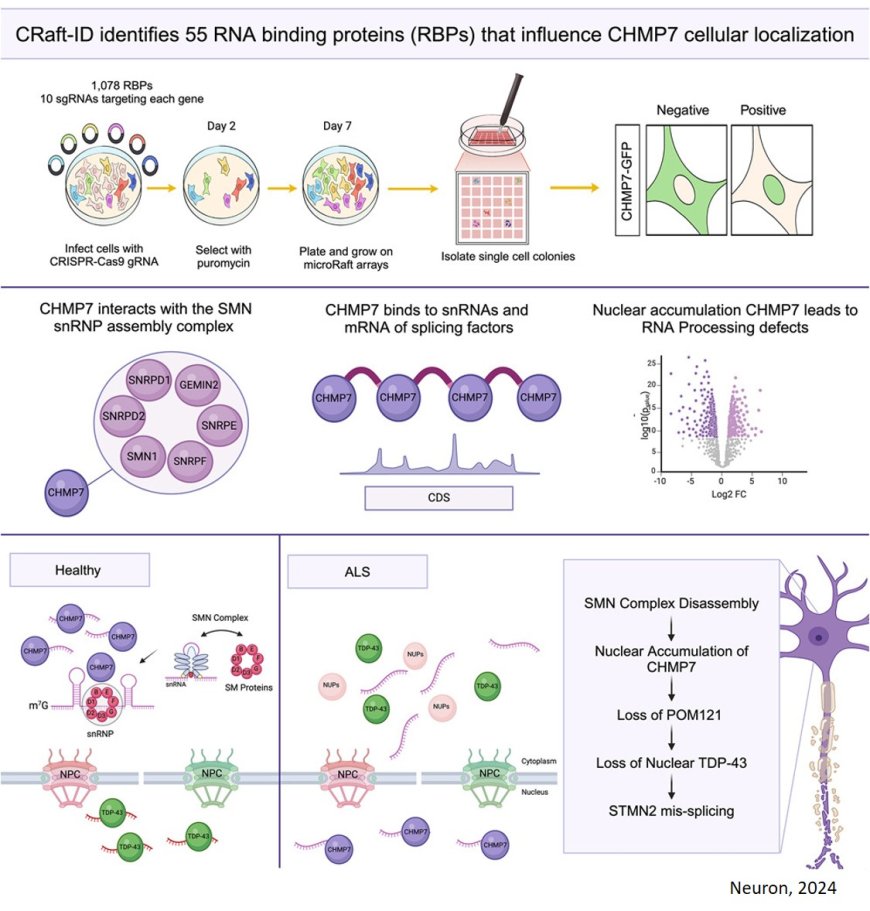
Now, researchers report that they have identified a key pathway that sets off neurodegeneration in the early stages of the disease. The findings could lead to development of therapies to prevent or slow the progression of ALS early on, before major damage has been done. The study was published in Neuron.
A protein called TDP-43 is usually located in the nucleus of motor neurons, where it regulates gene expression required for the cells to function. Studies have shown that when TDP-43 instead accumulates in the cytoplasm, outside of the nucleus, it is a telltale sign of ALS. How the protein ends up in the wrong place, leading to neuronal degeneration, has stumped researchers until now.
“By the time you see a patient with ALS and you see the TDP-43 protein aggregated in the cytoplasm, it's like the accident site with all the cars crashed already, but that's not the initiating event,” said the corresponding author.
Tracing the events leading up to the “accident”, the author explains that another protein, called CHMP7 — normally found in the cytoplasm — builds up in the nucleus instead, setting off a cascade of events that ultimately lead to motor neuron degeneration. But what causes CHMP7 to accumulate in the nucleus to begin with?
The team screened for RNA-binding proteins that might influence CHMP7 build-up in the nucleus. This yielded 55 proteins, 23 of which had a potential connection to ALS pathogenesis. Inhibiting the production of several of these proteins led to an increase in CHMP7 in the nucleus. Further experiments with motor neurons created from ALS-patient-derived induced pluripotent stem cells resulted in the surprising discovery that depleting one of these, an RNA-splicing associated protein called SmD1, which had not previously been known to affect CHMP7 levels, led to the largest uptick in its nuclear accumulation.
A build-up of CHMP7 in the nucleus damages nucleoporins, which the authors liken to tiny portals in the membrane separating the nucleus from the cytoplasm that orchestrate the movement of proteins and RNA between the two cellular spaces. Dysfunctional nucleoporins allow TDP-43 to exit the nucleus and accumulate in the cytoplasm. Once there, the protein can no longer oversee the gene expression programs necessary for neurons to function.
However, when the researchers boosted SmD1 expression in cells, CHMP7 was restored to its usual location in the cytoplasm, leaving nucleopores intact, allowing TDP-43 to stay in the nucleus, thus sparing the motor neurons from degeneration.
“You can actually fix the localization of this CHMP7 protein and therefore all of the downstream effects,” said the first author of the study.
What's more, the SmD1 protein is part of SMN, a multiprotein complex. SMN dysfunction is implicated in another neurodegenerative disorder, spinal muscular atrophy.
“We're intrigued because there are actually therapeutics for spinal muscular atrophy,” the senior author said. “One of them, risdiplam, is a small molecule compound that enhances the splicing and expression of SMN2, a gene closely related to the SMN1 gene that becomes dysfunctional in ALS.”
This hints at the possibility that using risdiplam to raise SMN levels could prevent ALS from developing past the earliest stage of the disease.
“It's not like all the neurons die at once,” said the author. “Some neurons die first, and then there is spread across other neurons. Perhaps as soon as you get symptoms, we could treat the patient so that the rest of the neurons don't crash and hope you stop the progression of ALS.”
The researchers think the SMN complex could play a crucial role in the onset of ALS, but further research is needed. The next steps will be to raise funds to continue the research in animal models and in other genetic models of ALS, and eventually test the effectiveness of risdiplam or other compounds for short-circuiting ALS.