Fiber consumption protects gut from serious bacterial infection

A study published in the journal Cell Host & Microbe, the researchers suggest that a diet rich in soluble fiber can protect the intestine against pathogenic bacteria.
The conclusion is based on experiments with mice exposed to Clostridioides difficile, which causes colon inflammation and diarrhea and affects about 500,000 people a year in the United States.
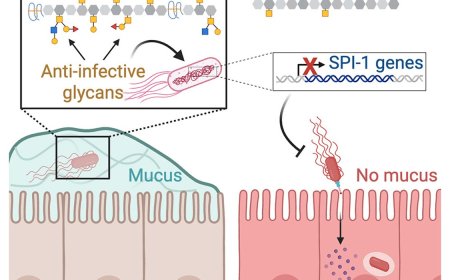
“We were able to treat the mice that had an infection with a diet supplemented with soluble fiber. This is digested by the intestinal microbiota, which produces compounds such as acetate. This initiates a cascade of interactions that leads to an appropriate immune response to deal with the infection,” explains the first author of the study.
The authors observed that the mice that consumed a diet rich in soluble fiber produced more acetate in the intestine. This increase helped regulate the immune response in the layer that covers the inner wall of the organ, known as the epithelium, making it effective in fighting the C. difficile bacteria.
Acetate is a short-chain fatty acid produced by the digestion of soluble fibers, a process carried out by the bacteria that live in the intestine.
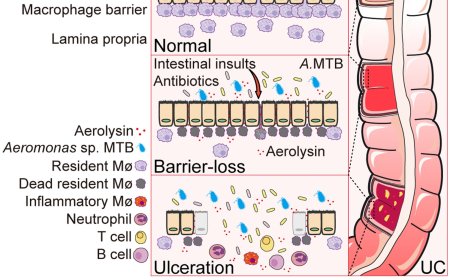
In the study, mice fed a low-fiber diet produced little acetate. As a result, the expression of components of the so-called major histocompatibility complex class 2 (MHC-II) was increased in the intestinal epithelium. Although MHC-II is an essential molecule in the defense against infection, its excessive production can cause exaggerated inflammation, which damages the tissues and worsens the patient’s condition.
“It’s a similar effect to what happens in severe COVID-19 when the immune response itself leads to tissue destruction and even death. In our study, the consumption of soluble fiber regulated this response,” says a co-author of the article.
Usually acquired by older hospitalized patients who have been treated with antibiotics, C. difficile infection causes severe diarrhea, which can lead to sepsis (generalized infection) and even death. Many strains are resistant to existing drugs, making treatment difficult.
In the animals treated in the study with a diet low in fiber and therefore low in acetate production, the immune response was exacerbated. The epithelial cells overproduced MHC-II, which has the function of presenting pathogen molecules (antigens) to activate CD4+ T lymphocytes, which are responsible for fighting infection.
Among these defense cells, intraepithelial lymphocytes (IELs) became over-activated and began releasing more inflammatory mediators, such as gamma-type interferon. The excess of these molecules intensifies the inflammation, causing more serious tissue damage and worsening the overall condition of the host, which can lead to death.
With the results of the mouse tests in hand, the researchers analyzed biopsies from patients who had been infected with C. difficile. As in the animals, the most severe cases had a higher presence of MHC-II and CD4+ T lymphocytes compared to the less severe cases.
“The study provides a broader understanding of the role of dietary fiber in the immune system. Although we’ve already shown the relationship between the production of short-chain fatty acids and immunity in other studies, this time we were able to demonstrate an unprecedented and coordinated event between the microbiota, the epithelium and the immune cells in the fight against infection,” comments the author.
https://www.cell.com/cell-host-microbe/fulltext/S1931-3128(24)00484-0
https://sciencemission.com/Fiber--and-acetate-mediated-modulation-of-MHC-II-expression