Gestational diabetes etiology and molecular mechanisms
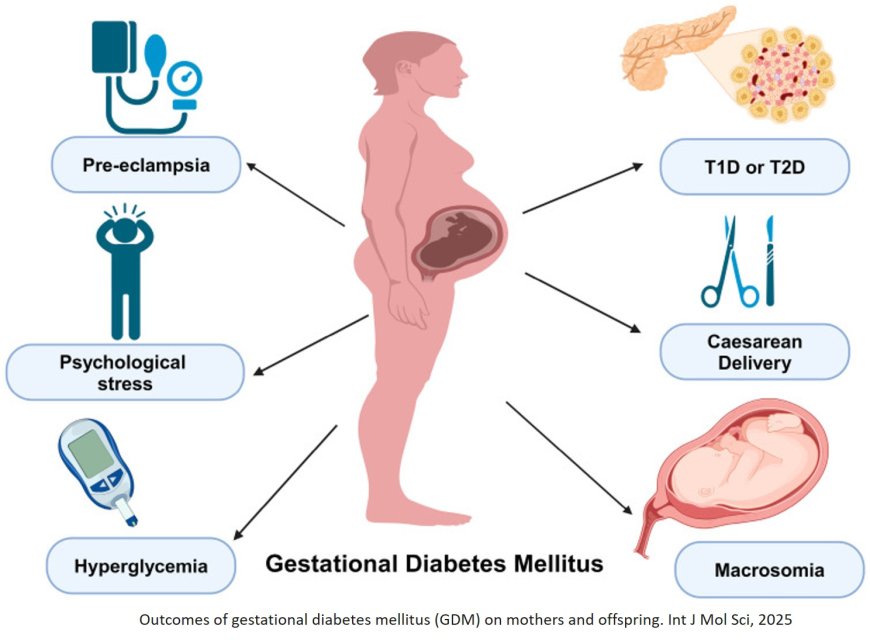
Gestational diabetes mellitus (GDM) is a condition characterized by high blood sugar levels that are first recognized during pregnancy. Here are the etiology and molecular mechanisms of GDM:
Etiology
1. Hormonal changes: During pregnancy, the placenta produces various hormones, such as human placental lactogen (hPL), progesterone, and cortisol, which can contribute to insulin resistance.
2. Insulin resistance: As pregnancy progresses, insulin sensitivity decreases, leading to insulin resistance.
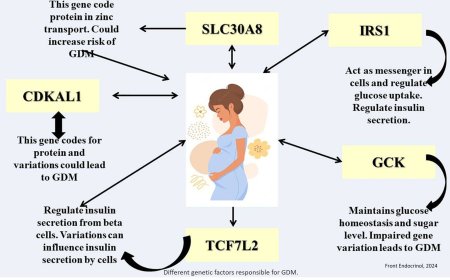
3. Genetic predisposition: Women with a family history of diabetes or GDM are more likely to develop GDM.
4. Obesity: Excess weight, particularly central obesity, can contribute to insulin resistance and GDM.
5. Ethnicity: Women from certain ethnic groups, such as Hispanic, African American, and Asian, are at higher risk of developing GDM.
Molecular Mechanisms
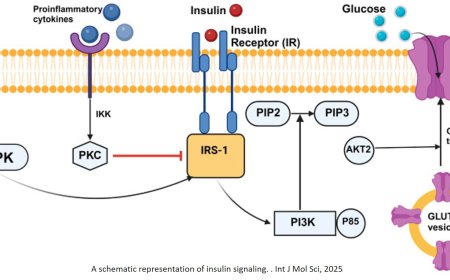
1. Insulin signaling pathway: Impaired insulin signaling, including reduced insulin receptor substrate-1 (IRS-1) phosphorylation, contributes to insulin resistance.
2. PI3K/AKT pathway: Altered PI3K/AKT signaling, including reduced phosphatidylinositol 3-kinase (PI3K) activity, contributes to insulin resistance.
3. Inflammation: Chronic inflammation, mediated by cytokines such as tumor necrosis factor-alpha (TNF-alpha) and interleukin-6 (IL-6), contributes to insulin resistance.
4. Adipokines: Altered adipokine secretion, including reduced adiponectin and increased leptin, contributes to insulin resistance.
5. Epigenetic changes: Epigenetic changes, such as DNA methylation and histone modification, can affect gene expression and contribute to insulin resistance.
Key Players
1. Insulin receptor: The insulin receptor plays a critical role in insulin signaling.
2. IRS-1: IRS-1 is a key substrate of the insulin receptor and plays a critical role in insulin signaling.
3. PI3K: PI3K is a key enzyme involved in insulin signaling.
4. AKT: AKT is a key protein involved in insulin signaling.
5. Adiponectin: Adiponectin is an adipokine that plays a critical role in insulin sensitivity.
Therapeutic Targets
1. Insulin sensitizers: Improve insulin sensitivity, such as metformin and thiazolidinediones.
2. Insulin secretagogues: Enhance insulin secretion, such as sulfonylureas and meglitinides.
3. Anti-inflammatory agents: Reduce inflammation, such as aspirin and anti-TNF-alpha agents.
4. Adipokine modulators: Modulate adipokine secretion, such as adiponectin and leptin.
Future Directions
1. Personalized medicine: Tailoring therapies to individual patients based on their genetic and phenotypic profiles.
2. Biomarkers: Identifying biomarkers to predict GDM and monitor disease progression.
3. Epigenetic therapies: Targeting epigenetic changes to improve insulin sensitivity and reduce inflammation.