Gene therapy for chronic pain?
A preclinical study uncovered a new gene therapy that targets pain centers in the brain while eliminating the risk of addiction from narcotics treatments, a breakthrough which could provide hope for the more than 50 million Americans living with chronic pain.
Dealing with chronic pain can feel like listening to a radio where the volume is stuck at maximum volume, and no matter what you do, the noise never seems to dull or lessen. Opioid medications, like morphine, work by turning down the volume, but they also affect other parts of the brain, sometimes leading to dangerous side effects or even addiction.
The potential new gene therapy is akin to a volume knob that only turns down the pain station and leaves everything else untouched, according to research published in Nature.
“The goal was to reduce pain while lessening or eliminating the risk of addiction and dangerous side effects,” said a co-senior author. “By targeting the precise brain circuits that morphine acts on, we believe this is a first step in offering new relief for people whose lives are upended by chronic pain.”
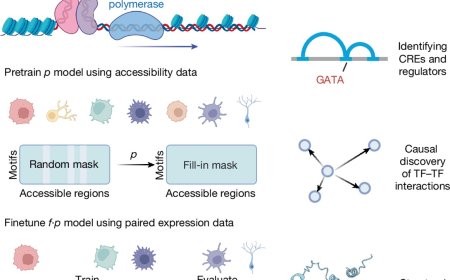
Morphine is a narcotic derived from opium with a high potential for abuse because patients who use it can develop tolerance, requiring higher and higher doses to achieve the same reduction in pain. By imaging brain cells that act as pain trackers, the team uncovered new insight into how morphine eases suffering.
From there, they built a mouse-model behavioral platform driven by artificial intelligence (AI) that tracks natural behaviors, creates a readout of pain levels, and helps gauge how much treatment is needed to alleviate the pain.
This readout, used as a sort of map, allowed the team to design a targeted gene therapy that mimics morphine’s beneficial effects but avoids its addictive ones while delivering an “off switch” specifically for pain felt in the brain. When activated, this switch provides durable pain relief without affecting normal sensation or triggering reward pathways that can lead to addiction.
“To our knowledge, this represents the world’s first CNS-targeted gene therapy for pain, and a concrete blueprint for non-addictive, circuit-specific pain medicine,” the author said.
Chronic pain, known to some as a ‘silent epidemic’ impacts approximately 50 million Americans, costing upward of $635 million annually in direct medical expenses and indirect costs from lost productivity, including missed work and reduced earning capacity. Now, these findings have the potential to help ease that pain—or, turning down the noise—for some, should the science hold through additional testing and into clinical trials.
https://www.nature.com/articles/s41586-025-09908-w
https://sciencemission.com/Mimicking-opioid-analgesia