High-salt diet inflames the brain and raises blood pressure
A new study finds that a high-salt diet triggers brain inflammation that drives up blood pressure.
The research suggests the brain may be a missing link in certain forms of high blood pressure – or hypertension – traditionally attributed to the kidneys.
“This is new evidence that high blood pressure can originate in the brain, opening the door for developing treatments that act on the brain,” said the senior author.
Hypertension affects two-thirds of people over 60 and contributes to 10 million deaths worldwide each year. Often symptomless, the condition increases the risk of heart disease, stroke and other serious health problems.
About one-third of patients don’t respond to standard medications, which primarily target the blood vessels and kidneys based on the long-standing view that hypertension begins there. The study, published in the journal Neuron, suggests the brain may also be a key driver of the condition, particularly in treatment-resistant cases.
To mimic human eating patterns, rats were given water containing two per cent salt, comparable to a daily diet high in fast food and items like bacon, instant noodles and processed cheese.
The high-salt diet activated immune cells in a specific brain region, causing inflammation and a surge in the hormone vasopressin, which raises blood pressure. Researchers tracked these changes using cutting-edge brain imaging and lab techniques that only recently became available.
Microglia phagocytose astrocytic processes, reducing astrocytic coverage of vasopressin neurons. The pruning of astrocytic processes impairs synaptic glutamate clearance, enabling activation of extrasynaptic glutamate NMDA receptors and increasing the activity of vasopressin neurons.
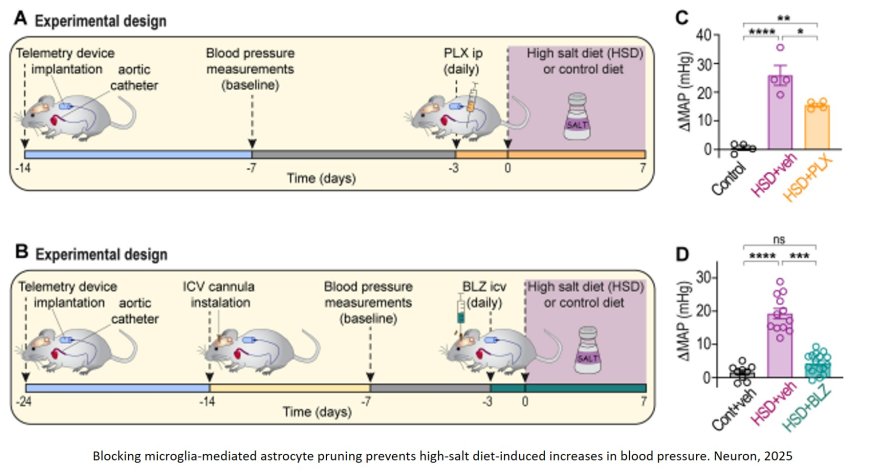
Inhibiting microglia-mediated astrocyte pruning attenuates the increased neuronal activity and vasopressin-dependent hypertensive phenotype of rats fed a high-salt diet. Thus, microglia orchestrate neuron-glia interactions and regulate neuronal activity through astrocyte pruning.
“The brain’s role in hypertension has largely been overlooked, in part because it’s harder to study,” the author said. “But with new techniques, we’re able to see these changes in action.”
The researchers used rats instead of the more commonly studied mice because rats regulate salt and water more like humans. That makes the findings more likely to apply to people, noted the author.
Next, the scientists plan to study whether similar processes are involved in other forms of hypertension.












