Key mechanism of brain repair in vascular dementia
A new study has uncovered how inflammation in brain blood vessels exacerbates damage in vascular dementia and demonstrated that targeting this process with a repurposed drug can promote brain repair and functional recovery in mice.
Published in Cell, the research combines laboratory and human data to pinpoint a critical signaling pathway that could lead to the first effective treatment for this understudied form of dementia.
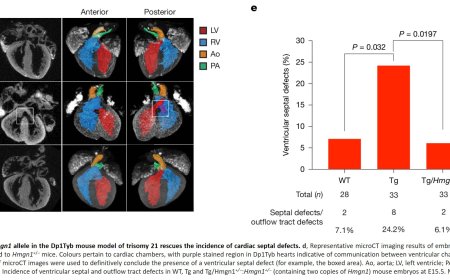
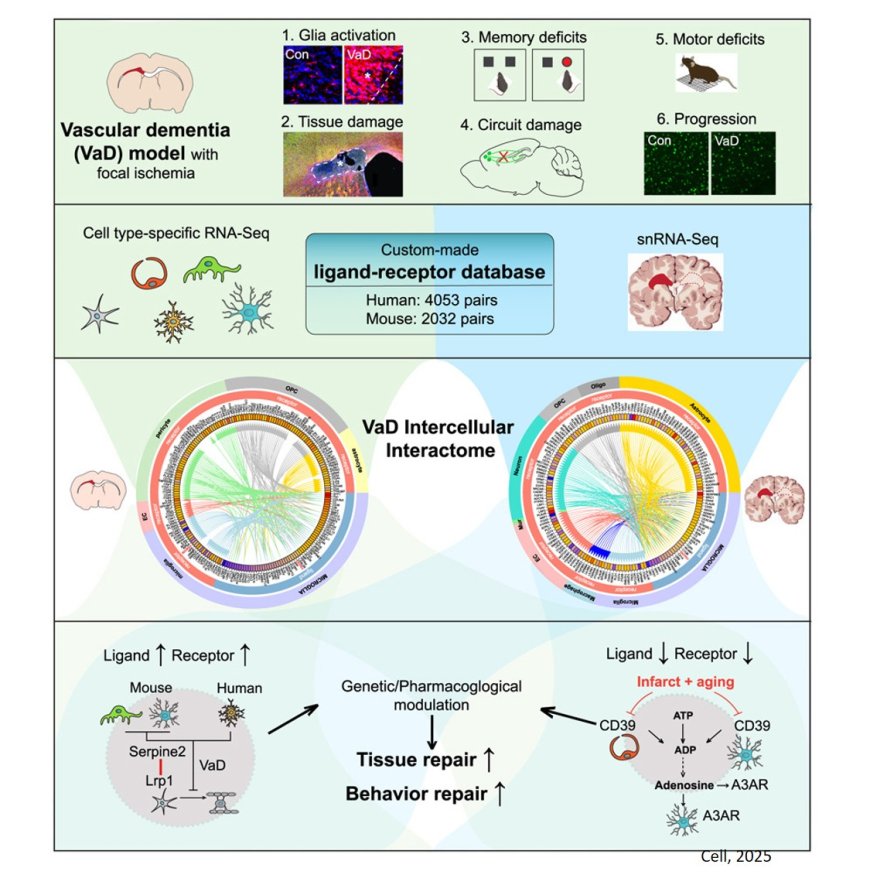
Vascular dementia is the second leading cause of dementia. This disease co-occurs with Alzheimer’s disease in the leading cause of dementia, termed “mixed dementia.” There is no drug therapy that promotes recovery in vascular dementia. A key problem in this disease is that the brain damage expands from initial areas, to become larger over time. The team sought to identify what happens in the brain in these areas of expansion. To do this, the researchers identified all the molecules that communicate among the cells of the brain adjacent to the dementia lesions, and which ones are abnormally up or down in the disease compared to normal brain. By doing this both in laboratory models of vascular dementia and in human brain, the team was able to precisely identify the “interactome” in vascular dementia — all the molecules that signal or interact in the cells at risk.
“We reasoned that the cell in the brain areas in which the disease expands will lose their normal signaling with each other. In other words, the cell-to-cell interaction is disturbed in a toxic way in vascular dementia. We set out to identify these cell-to-cell interactions or the “interactome” in vascular dementia,” said the study’s lead author.
One molecular system jumped out as potentially significant. This system communicates between blood vessel cells and adjacent brain inflammatory cells, termed microglia. In vascular dementia, the CD39 (an enzyme) and the adenosine A3 receptor (A3AR) are downregulated together in these two cell types, synergistically by aging and vessel ischemic lesion. Because vascular dementia is a disease of aging, this double finding — a downregulation with both disease and aging — signaled a possibly significant role. CD39 generates through several steps the molecule adenosine, which binds to A3AR, and modifies inflammation, downregulating some of its harmful effects.
To test this CD39/A3AR system as a possible drug target for treating vascular dementia, the group utilized a drug that is in clinical trials for psoriasis. When given to mice in a model of vascular dementia, this drug promoted repair of brain tissue and recovery of memory and gait functions.
“The most exciting finding was that delayed intervention still worked,” said the lead author. “This is crucial because vascular dementia is often diagnosed late. By targeting the crosstalk between blood vessels and brain cells, we’re addressing the root cause of damage, not just masking symptoms.”
While the results are promising, further studies are needed before human trials can begin. The team is now optimizing dosing and exploring biomarkers to track the therapy’s effectiveness.