How thalamus governs our state of consciousness
In hospital operating rooms and intensive care units, propofol is a drug of choice, widely used to sedate patients for their comfort or render them fully unconscious for invasive procedures.
Propofol works quickly and is tolerated well by most patients when administered by an anesthesiologist.
But what’s happening inside the brain when patients are put under and what does this reveal about consciousness itself?
Investigators are studying the nature of consciousness, have successfully used the drug to identify the intricate brain geometry behind the unconscious state, offering an unprecedented look at brain structures that have traditionally been difficult to study.
“Consciousness has been the subject of study from various perspectives and understanding the neurobiological foundations of consciousness carries major implications of multiple medical disciplines such as neurology, psychiatry and anesthesiology,” said the author.
To date, researchers have debated about how anesthetics suppress consciousness.
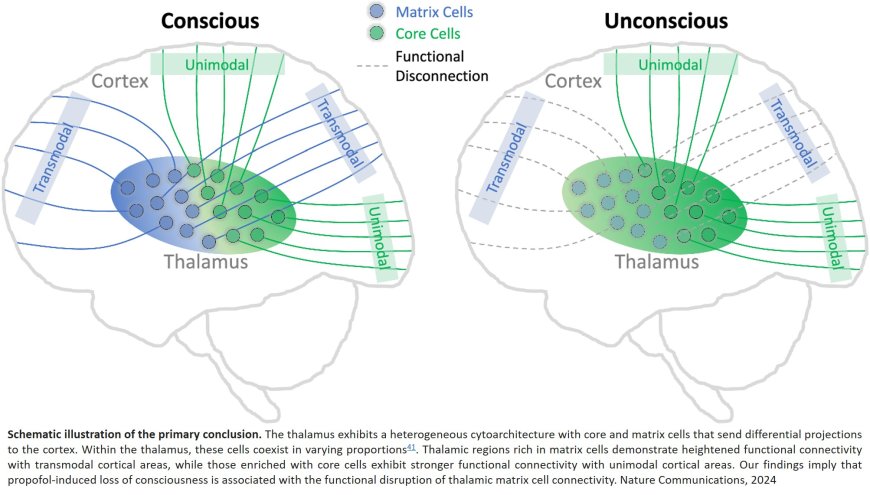
Specifically, whether the site of action lies primarily in the thalamus, an egg-shaped structure deep within the brain, which receives information from what we see, touch and hear, or in the cerebral cortex, which processes that information in complex ways.
A study published in the journal Nature Communications outlines for the first time in humans how the connections among brain cells within those two important areas are modified by propofol.
In healthy volunteers, they mapped changes in the brain’s architecture before, during and after propofol sedation, guided by functional magnetic resonance imaging.
This enabled them to monitor blood flow to areas of the brain as the study participants entered and exited an unconscious state.
At baseline, explains the author, the thalamus has a balanced level of activity of both specific nuclei (clusters of brain cells) that send sensory information to highly defined areas of the cortex—known as unimodal processing—and nonspecific nuclei that send information more diffusely throughout a higher layer of the cortex, known as transmodal processing.
The team found that, under deep sedation, the thalamus showed a drastic reduction in activity in clusters of brain cells responsible for transmodal processing leading to a dominant unimodal pattern—suggesting that while sensory inputs are still received, there is no integration of those inputs.
“The field has been focusing on anesthetic effects in the thalamus and cortex for more than two decades—I believe this study significantly advances the neurobiology,” said the senior author.
Next, they discovered the specific cell types that played a role in the shift to an unconscious state and their relationship to the change in thalamic processing.
The thalamus contains at least two distinct cell types, says the lead, which are core cells and matrix cells.
“We now have compelling evidence that the widespread connections of thalamic matrix cells with higher order cortex are critical for consciousness,” said another author.
Imagining that the cortex is layered like an onion, core cells connect to lower layers while matrix cells connect to higher layers in a more spread out manner.
By measuring mRNA expression signatures—like I.D. badges for the cells—they were able to see that a disruption in the activity of matrix cells played a greater role in the transition to unconsciousness than core cells.
An additional surprise was that GABA, a major inhibitory transmitter in the brain usually thought to be key to propofol’s actions, didn’t appear to play as prominent a role as expected.
“The results suggest that loss of consciousness during deep sedation is primarily associated with the functional disruption of matrix cells distributed throughout the thalamus,” said the lead.