Prime editing treats childhood brain hemiplegia in mice
By the time they are a few months old, infants born with alternating hemiplegia of childhood (AHC) begin experiencing terrifying episodes of paralysis and seizures, and will soon show developmental delays and intellectual disability. There is no cure or effective treatment for this rare genetic disease, but new research suggests a potential path to one.
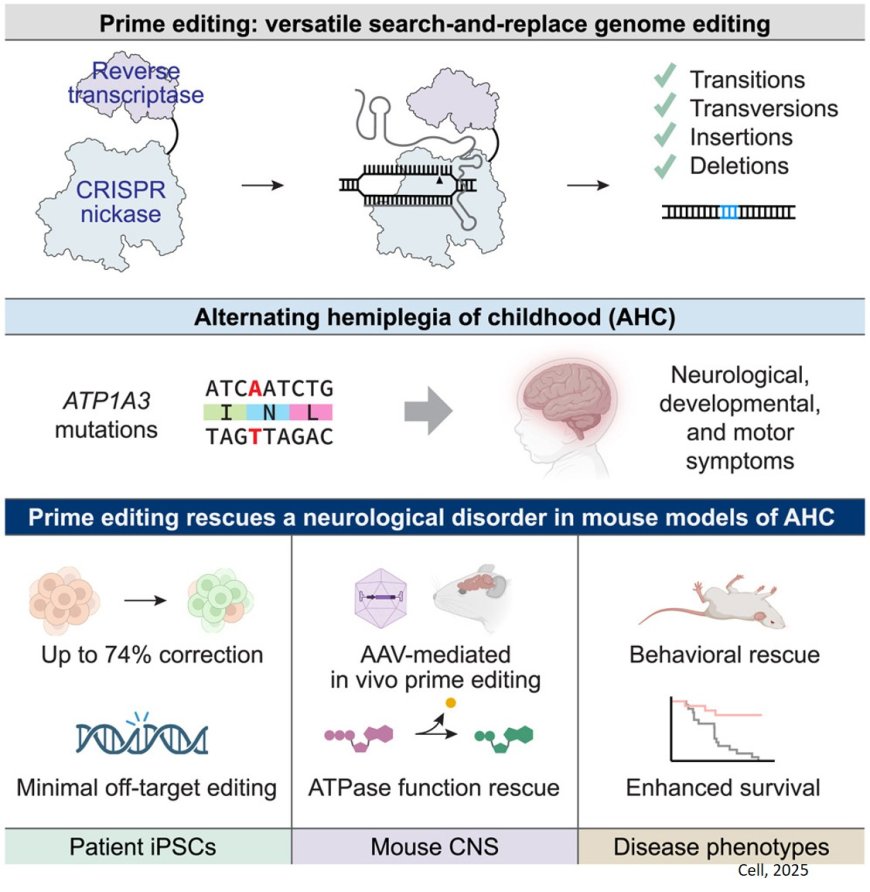
Researchers have used prime editing, a precise and versatile form of gene editing, to correct the root cause of AHC in mice. The team used a scalable approach to develop prime editing treatments that directly repaired five different AHC-causing genetic mutations. Mice that received the treatment had far fewer and less severe symptoms of AHC, and survived more than twice as long as untreated mice.
The new study, published in Cell, is the first time prime editing has been used to treat a neurological disease in animals, offering hope for treating people with AHC and other genetic brain disorders. The technology has already been successfully tested in a clinical trial for another rare genetic disease.
“This study is an important milestone for prime editing and one of the most exciting examples of therapeutic gene editing to come from our team,” said the senior author. “It opens the door to one day repairing the underlying genetic causes of many neurological disorders that have long been considered untreatable.”
The ability to precisely edit DNA directly in the brain has important implications for neurological diseases, said a co-senior author of the study. “This level of editing efficiency in the brain is really quite remarkable.”
The team’s patient partner is RARE Hope (formerly Hope for Annabel), a non-profit focused on accelerating research on AHC and developing scalable, patient-centric research platforms to benefit the larger rare disease community. RARE Hope initiated the collaboration and was closely engaged throughout the project.
The vast majority of AHC cases are caused by one of four mutations in ATP1A3, a gene essential for brain cell function. In the new work, the team set out to simultaneously develop prime editing treatments that could fix five ATP1A3 mutations, including the four most common — a scale rarely attempted in therapeutic gene editing research.
Most other gene editing treatments are designed to correct one mutation at a time. The scientists worked on correcting all five mutations, streamlining experiments, saving resources, and testing the robustness of the underlying science.
“We developed a robust framework to correct multiple mutations in parallel,” said one of three co-first authors. “This effort was really about creating a blueprint that could be rapidly applied to other rare diseases too.”
The researchers first tested their strategies in cultured cells from patients with AHC. They demonstrated that they could correctly repair AHC mutations in up to 90 percent of treated cells, with minimal changes to other stretches of DNA.
Next, the group tested their treatments in two mouse models of AHC, which carry Atp1a3 mutations similar to those in patients with AHC. Without treatment, the mice developed seizures, movement problems, and died prematurely. When the scientists injected their editing system into the brains of the animals, their symptoms disappeared or were substantially reduced. Treated mice survived more than twice as long as untreated animals.
Moreover, the function of their Atp1a3 protein was restored in the brain, and their motor and cognitive deficits were ameliorated. The scientists delivered the prime editors to cells in mice using clinically validated viruses called AAVs, which are already used in FDA-approved gene therapies targeting brain cells.
The team also tested traditional gene therapy, which delivered an extra, healthy copy of the ATP1A3 gene to cells, and found that symptoms did not improve in animals. This finding highlights the unique advantage of using gene editing to directly correct a mutation that results in a malfunctioning, disease-causing protein, the researchers said.
Because the treatment required direct injection into the brain shortly after birth, the team is now exploring less invasive delivery methods, and whether treatment later in life could still be effective.
Beyond AHC, the team sees their approach as a template for tackling other rare genetic diseases — especially those that affect the brain. With the ability to rapidly design and test multiple gene editing treatments at once, they hope to bring the same precision and speed to many other conditions.