Type 1 diabetes cured in mice with gentle blood stem-cell and pancreatic islet transplant
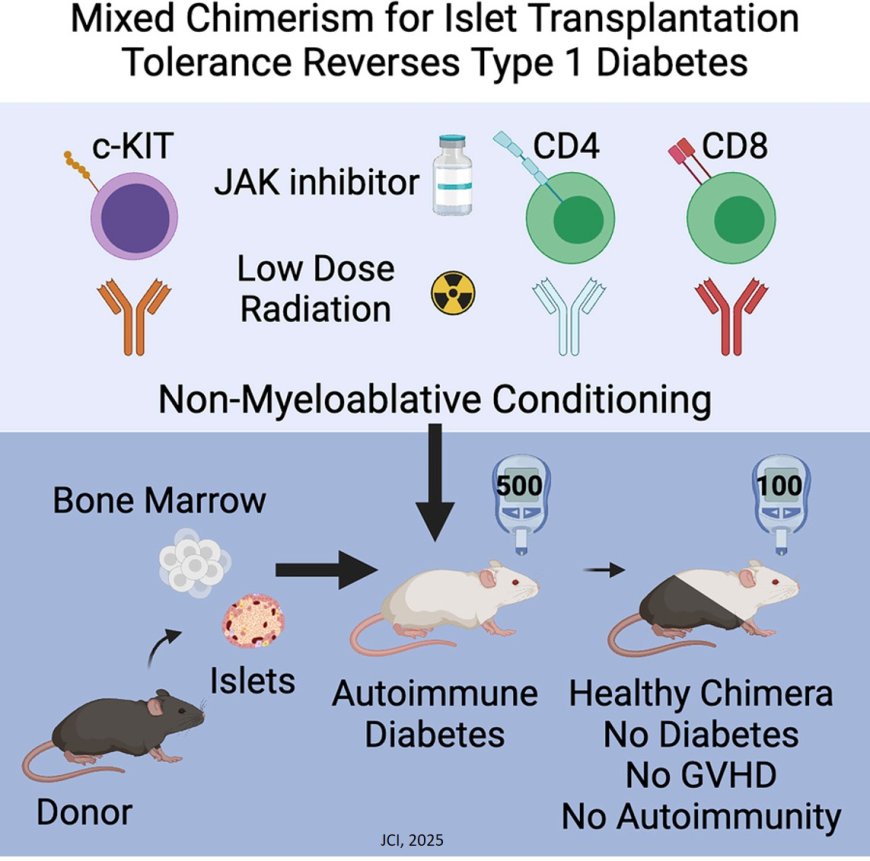
A combination blood stem cell and pancreatic islet cell transplant from an immunologically mismatched donor completely prevented or cured Type 1 diabetes in mice in a new study. Type 1 diabetes arises when the immune system mistakenly destroys insulin-producing islet cells in the pancreas.
None of the animals developed graft-versus-host disease — in which the immune system arising from the donated blood stem cells attacks healthy tissue in the recipient — and the destruction of islet cells by the native host immune system was halted. After the transplants, the animals did not require the use of the immune suppressive drugs or insulin for the duration of the six-month experiment.
“The possibility of translating these findings into humans is very exciting,” said the senior author. “The key steps in our study — which result in animals with a hybrid immune system containing cells from both the donor and the recipient — are already being used in the clinic for other conditions. We believe this approach will be transformative for people with Type 1 diabetes or other autoimmune diseases, as well as for those who need solid organ transplants.”
The study was which published in the Journal of Clinical Investigation.
The researchers in the previous study induced diabetes in mice by destroying insulin-producing cells in the pancreas with toxins. They then cured them with a gentle pre-transplant treatment of immune-targeting antibodies and low-dose radiation, followed by transplantation of blood stem and islet cells from an unrelated donor.
The current study tackled a more complex problem: curing or preventing diabetes caused by autoimmunity, in which the immune system spontaneously destroys its own islet cells. In people this is called Type 1 diabetes. Unlike in the induced-diabetes study — in which the researchers’ goal was to prevent the recipient’s immune system from rejecting donated islet cells — the transplanted islet cells in the autoimmune mice have two targets on their backs: Not only are they foreign, but they are vulnerable to autoimmune attack by a misguided immune system bent on destroying islet cells regardless of their origin.
“Just like in human Type 1 diabetes, the diabetes that occurs in these mice results from an immune system that spontaneously attacks the insulin-producing beta cells in pancreatic islets,” the author said. “We need to not only replace the islets that have been lost but also reset the recipient’s immune system to prevent ongoing islet cell destruction. Creating a hybrid immune system accomplishes both goals.”
Unfortunately, the inherent features that lead to autoimmune diabetes in these mice also make them more challenging to prepare for a successful blood stem cell transplant.
The solution the researchers found was relatively simple: the authors added a drug used to treat autoimmune diseases to the pre-transplant regimen the researchers had discovered in 2022. Doing so, then transplanting blood stem cells, resulted in an immune system made up of cells from both the donor and the recipient and prevented development of Type 1 diabetes in 19 out of 19 animals. Additionally, nine out of nine mice that had developed long-standing Type 1 diabetes were cured of their disease by the combined blood stem cell and islet transplantation.
Because the antibodies, drugs and low-dose radiation the researchers administered to the mice are already used in the clinic for blood stem cell transplantation, the researchers believe that translating the approach to people with Type 1 diabetes is a logical next step.
The earlier studies have shown that a bone marrow transplant from a partially immunologically matched human donor allowed formation of a hybrid immune system in the recipient, and subsequent long-term acceptance of a kidney transplant from the same donor. In some cases, the researchers showed that transplanted donor kidney function lasted for decades, without the need for drugs to suppress rejection.
A blood stem cell transplant can be used to treat cancers of the blood and immune system, such as leukemia and lymphoma. But in those settings, high doses of chemotherapy drugs and radiation needed to treat the cancer and replace the recipient blood and immune system often result in severe side effects. The researchers have devised a safer, gentler avenue to prepare recipients with non-cancerous conditions such as Type 1 diabetes for donor blood stem cell transplantation — knocking their bone marrow back just enough to provide a foothold for the donated blood stem cells to settle in and develop.
“Based on many years of basic research by us and others, we know that blood stem cell transplants could also be beneficial for a wide range of autoimmune diseases,” the author said. “The challenge has been to devise a more benign pre-treatment process, diminishing risk to the point that patients suffering from an autoimmune deficiency that may not be immediately life-threatening would feel comfortable undergoing the treatment.”
“Now we know that the donated blood stem cells re-educate the recipient animal’s immune system to not only accept the donated islets, but also not attack its healthy tissues, including islets,” the author said. “In turn, the donated blood stem cells and the immune system they produce learn to not attack the recipient’s tissues, and graft-versus-host disease can be avoided.”
Challenges remain using this approach to treat Type 1 diabetes. Pancreatic islets can be obtained only after death of the donor, and the blood stem cells must come from the same person as the islets. It is also unclear whether the number of islet cells typically isolated from one donor would be enough to reverse established Type 1 diabetes.
But the researchers are working on solutions, which could include generating large numbers of islet cells in the laboratory from pluripotent human stem cells, or finding ways to increase the function and survival of transplanted donor islet cells.
In addition to diabetes, the authors expect that the gentler pre-conditioning approach they developed could make stem cell transplants a viable treatment for autoimmune disease such as rheumatoid arthritis and lupus, and non-cancerous blood conditions like sickle cell anemia (for which current blood stem cell transplant methods remain harsh), or for transplants of mismatched solid organs.
“The ability to reset the immune system safely to permit durable organ replacement could rapidly lead to great medical advances,” the author said.