A microbial molecule disarms inflammation and protects against diabetes
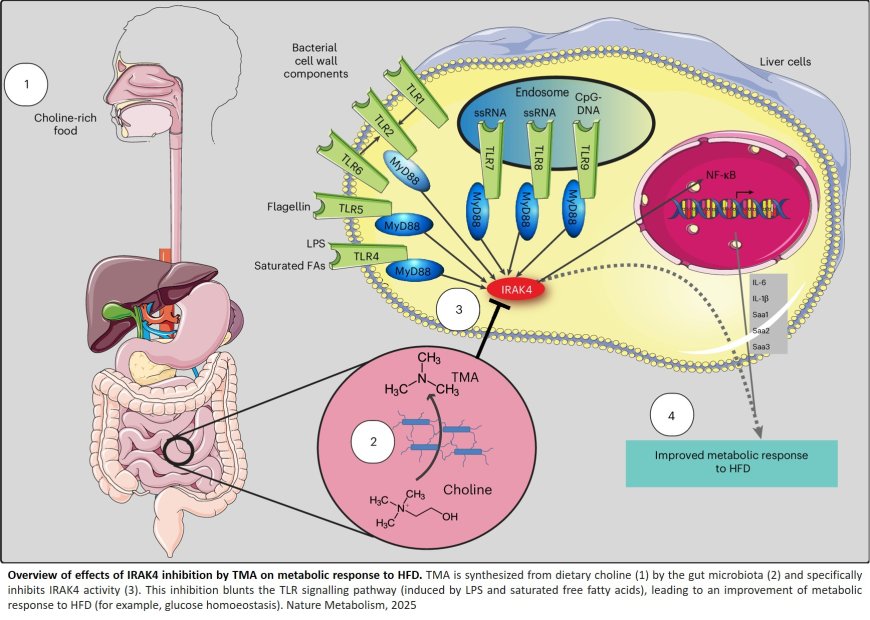
An international research team has uncovered a surprising ally in the fight against insulin resistance and type 2 diabetes: a microbial metabolite called trimethylamine (TMA). Published in Nature Metabolism, the study reveals that TMA, produced by gut bacteria from dietary choline can block a key immune pathway and improve blood sugar control.
This major breakthrough has its roots 20 years earlier. During his postdoctoral research, a researcher discovered that a high-fat diet leads to the presence of bacterial components in the body, which activates the immune system and triggers inflammation, eventually causing insulin resistance in diabetic individuals. Considered far-fetched in 2005, this finding is now well established and widely accepted by scientists.
In 2025, researchers finally uncovered how to counter this process. They observed that TMA, produced by gut bacteria from a natural nutrient, dietary choline, found in certain foods can improve blood-sugar control.
How? By acting as a natural inhibitor of the protein IRAK4, a key component of the immune system. Normally, when exposed to a high-fat diet, IRAK4 sounds the alarm and triggers inflammation to signal dietary imbalance.
The problem? With constant overload (as seen in type 2 diabetes), IRAK4 overreacts, causing cascading inflammation that drives insulin resistance.
By combining human cell models, mouse studies, and molecular-target screening, scientists discovered that TMA can bind directly to IRAK4 and block its activity. The direct effect is a reduction in fat-induced inflammation and a restoration of insulin sensitivity. In essence, it reprograms the negative metabolic responses caused by poor diet. Even more striking: the molecule can prevent sepsis-induced mortality in mice by blocking widespread inflammation.
“This shows how nutrition and our gut microbes can work together by producing molecules that fight inflammation and improve metabolic health!”, said a co-senior author.
The team also observed that genetically deleting IRAK4 or blocking it pharmacologically reproduced the beneficial effects of the bacterial metabolite. This opens new therapeutic avenues for diabetes, using a target, IRAK4, that is already validated within the pharmaceutical industry.
“This flips the narrative,” said the author. “We’ve shown that a molecule from our gut microbes can actually protect against the harmful effects of a poor diet through a new mechanism. It’s a new way of thinking about how the microbiome influences our health.”
“This shows how nutrition and our gut microbes can work together by producing molecules that fight inflammation and improve metabolic health!”, said the co-senior author.