Changes in microbiome predict risk for sexually transmitted disease
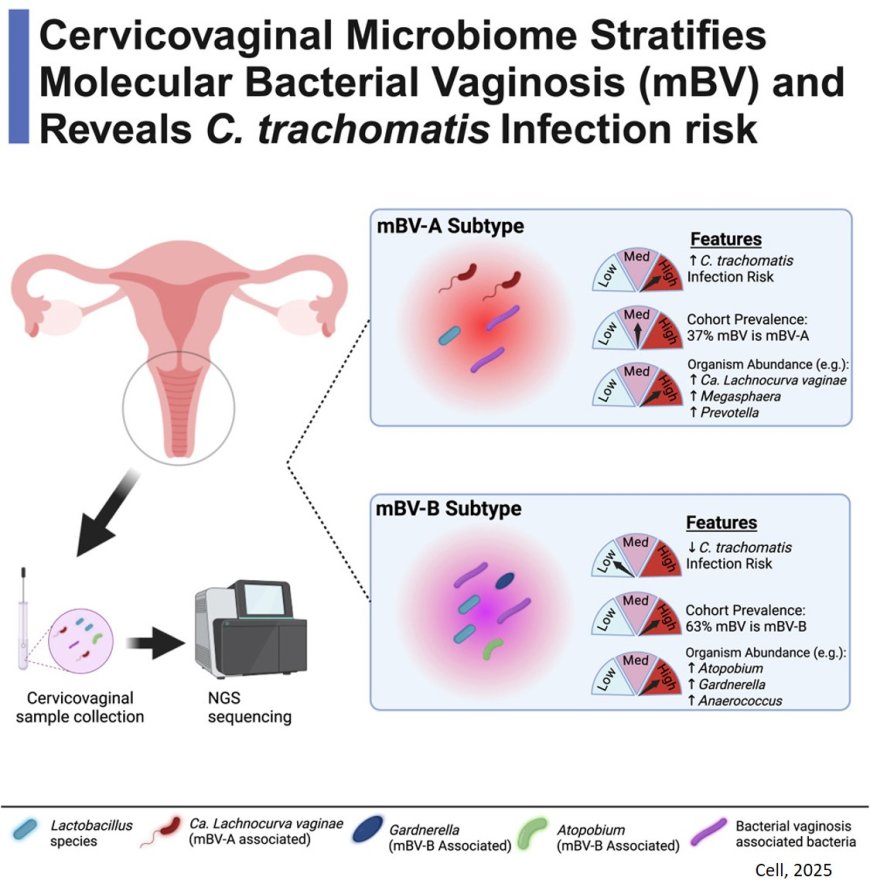
Women who develop bacterial vaginosis (BV) often later acquire chlamydia, a common and potentially serious sexually transmitted bacterial infection. Now, researchers have found that BV actually consists of two subtypes—one of which significantly increases the risk of developing chlamydia infections. The findings were made in a population of young Black and Hispanic women, who are disproportionately affected by both BV and chlamydia, but are historically understudied. The study, one of the largest and most comprehensive of its kind, was published in the journal Cell.
“It was already known that BV raises a woman’s risk for acquiring chlamydia, but it wasn’t clear how the microbiome imbalances seen in BV contribute to that risk,” said study co-leader. “This research shows that specific changes in the cervicovaginal microbiome set the stage for chlamydia. And it shows that targeting treatment against the more-dangerous BV subtype could potentially prevent many women from developing chlamydia, which is particularly prevalent in historically underserved communities.”
BV affects at least 30% of women at any given time and up to 50% of Black and Hispanic women. Black and Hispanic adolescent and young adult females have a five-fold higher risk of acquiring chlamydia compared with their white counterparts.
“This study was made possible by the participation of young women of color, who are at highest risk for this infection and most likely to experience its negative impact,” said the study co-author. “We hope that our research and future studies continue to address disparities in healthcare, improve access to treatment, and enhance our approach to personalized care.”
BV is caused by imbalances in the cervicovaginal microbiome—the collection of bacteria naturally found in the genital tract. Common symptoms include vaginal discharge, itching or irritation, and burning sensation during urination, although many cases are asymptomatic. BV can be readily treated with antibiotics.
In the new study, the researchers used advanced DNA-sequencing technology to analyze the cervicovaginal microbiomes of 560 adolescent and young adult Black and Hispanic females. The analyses were performed before infection with chlamydia, at the time of infection, and following antibiotic treatment, allowing the researchers to identify which combination of cervicovaginal bacteria is associated with subsequent chlamydia infections.
The analysis detected two distinct subtypes of BV. One subtype—a collection of ten different interconnected bacterial types that account for about 40% of all BV cases—contributed to increased risk for acquiring chlamydia, subsequent reinfection with chlamydia, and complications such as pelvic inflammatory disease.
“This study adds to the growing evidence of the impact of BV on the risk of clinically significant infections, including chlamydia and human papillomaviruses, that can cause cervical cancer,” said a co-author. “It’s our hope that this work to reveal the connections between the cervicovaginal microbiome, common infections like chlamydia and HPV, and cancer might help advance the larger effort to prevent more cancers and other resulting conditions.”
Detecting and treating these infections could substantially reduce the incidence of chlamydia and its serious consequences including pelvic inflammatory disease, infertility, and miscarriage. The findings also suggest that altering the cervicovaginal microbiome could be a strategy for both treating BV and preventing chlamydia.”
At present, advanced cervicovaginal microbiome analysis is not available to most clinicians. But, the author said, “I can envision a scenario where it would be readily accessible to most doctors and perhaps even incorporated into home tests, like we have now for COVID-19.”
“This study represents a breakthrough by showing that the risk posed by a relatively benign bacterial condition such as BV can be assessed through microbiome analysis,” said the first author of the paper. “Our findings suggest that only a subset of BV cases may require treatment to prevent subsequent infections with chlamydia.”