Gene therapy for alpha thalassemia major
Thanks to groundbreaking in-utero blood transfusion technology, what was once a fatal diagnosis in the womb can now result in live births. However, this medical advancement created a new challenge: a growing population of children born with that diagnosis — the severe, inherited blood disorder alpha thalassemia — which requires lifelong specialized care.
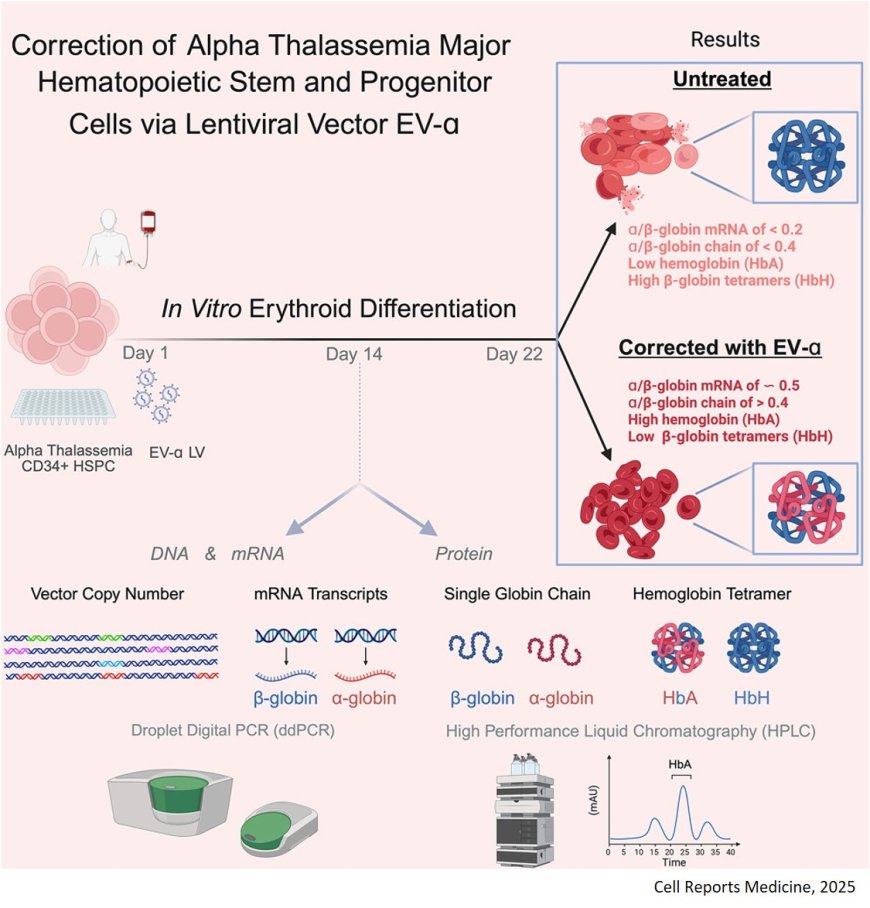
But a research team is developing a one-time stem cell gene therapy treatment for this condition that’s potentially curative. The study findings are detailed in Cell Reports Medicine.
Individuals born with alpha thalassemia major are missing all four copies of the genes required to produce hemoglobin. Without hemoglobin to carry oxygen in the blood, patients face serious health issues, including a lifelong dependence on blood transfusions, severe organ damage and early death due to iron overload.
While a bone marrow transplant from a matched donor could be curative, finding a compatible donor is often difficult, and the procedure carries the risk of graft versus host disease, a life-threatening condition in which transplanted cells attack the recipient’s body.
The research team’s gene therapy eliminates both challenges.
Instead of relying on donor cells, the therapy involves collecting a patient’s own blood stem cells, adding the missing alpha-globin gene, and then returning the corrected cells back to the patient.
“The idea of a blood stem cell gene therapy is to fix the disease at the DNA level,” said first author.
To get the alpha-globin gene into the DNA of patient cells, the researchers use a viral vector — a modified virus that has the unique ability to deliver genetic information into a cell’s nucleus without causing infection.
In alpha thalassemia major patient cells, the gene therapy successfully restored normal alpha-globin protein production to healthy levels, enabling the modified cells to produce functional hemoglobin.
“More babies with alpha thalassemia major are surviving birth than ever before, thanks to in-utero blood transfusions,” the senior author said. “Now we’re working to give them the chance at a completely normal life, free from a lifetime of medical dependence.”
https://www.cell.com/cell-reports-medicine/fulltext/S2666-3791(25)00435-5
https://sciencemission.com/globin-expression-in-%CE%B1-thalassemia