How altered expression of Presenilin2 impacts Alzheimer’s disease-relevant brain circuits
Alzheimer’s disease is a debilitating condition that slowly robs people of their memory and cognitive abilities, affecting millions of people worldwide. Familial Alzheimer’s disease (FAD), a rare inherited form of the disease, is linked to mutations in several genes, including APP, PSEN1, and PSEN2. The impact of PSEN2 mutations has remained less understood—until now.
A research team has shed light on how mutated PSEN2 accelerates disease progression in FAD. Their findings, published in Nature Communications, offer new insights into the mechanisms driving this genetic form of the disease.
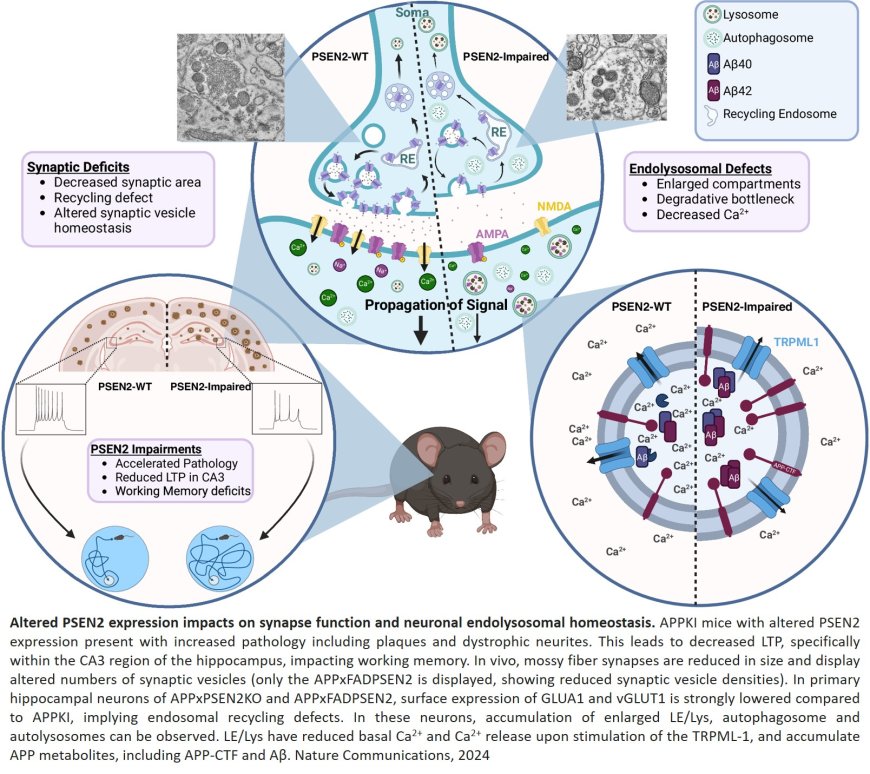
Alzheimer’s disease is characterized by the gradual loss of cognitive function, memory, and behavioral changes, with the brain showing a build-up of amyloid plaques. These plaques form after a protein called APP (amyloid precursor protein) is “cut into pieces” by, among others, the γ-secretase complex. Some of these pieces are β-amyloid (Aβ) peptides, which can clump together to form the harmful plaques. The γ-secretase complex exists in different variants, containing either PSEN1 or PSEN2, which actually impacts its location within the cell, hinting at subtle functional differences between the two. Mutations in the genes encoding these functionally related proteins can cause FAD, an inherited form of Alzheimer’s that typically develops earlier than the more common late-onset version, with symptoms sometimes starting as early as a person's 30s or 40s.
Although it is known that toxic Aβ fragments build up early in FAD and contribute to brain damage, the specific mechanisms by which PSEN2 mutations accelerate this process were not fully understood. The lab compared the effects of a loss of PSEN2 with those of a mutant form of the PSEN2 gene to understand how disease develops in these FAD cases.
The research team studied the effects of PSEN2 loss and an FAD-linked mutation in mouse models mimicking Alzheimer’s disease. Both the absence of PSEN2 and the presence of mutated PSEN2 led to faster accumulation of amyloid plaques in the brain. Moreover, the mice with no or mutated PSEN2 both exhibited significant memory impairments. These impairments correlated with structural and functional changes in the hippocampus, a key area for working memory that is primarily affected in AD patients. This brain area is essential for tasks like remembering directions while driving or walking, or following multi-step instructions, such as cooking recipes.
Consistently, the researchers observed that missing or impaired PSEN2 harmed the functioning of synapses—the connections between brain cells that allow them to communicate. The ability of synapses to strengthen over time, a process known as long-term potentiation, was impaired as well, which negatively affects learning and memory.
To uncover the origin of these impairments, the team investigated mechanisms within crucial brain cells—neurons. They found that PSEN2 plays a critical role in maintaining healthy cellular processes within late endosomes and lysosomes—the cells’ “garbage disposal system” that breaks down and recycles proteins. A lost or mutated PSEN2 gene disrupted these processes, causing a toxic build-up of APP fragments within, including Aβ peptides. So not only does impairment of the PSEN2 gene lead to more toxic amyloid plaques, it also leads to a degradative bottleneck within nerve cells, causing defects in the recycling of other molecules, including those that are responsible for transmitting signals between nerve cells.
“These results highlight the multi-faceted impact of PSEN2 mutations—on one hand, driving toxic amyloid accumulation, and on the other, impairing fundamental cellular maintenance systems, amplifying synaptic and cognitive decline”, says the first author of the paper.
The senior author emphasizes: “Our findings underscore the importance of PSEN2 in regulating brain cell health. Targeting the underlying cellular dysfunction caused by PSEN2 mutations could be a potential route for Alzheimer’s treatments. To translate these insights into treatments, we require further research, but our work suggests that therapies aimed at restoring the function of endosomes and lysosomes or normalizing γ-secretase activity in these organelles could help mitigate the effects of PSEN2 mutations and slow disease progression in FAD.”