Epigenetic changes can cause type 2 diabetes
Do epigenetic changes cause type 2 diabetes, or do the changes occur only after a person has become ill? A new study by researchers provides increased support for the idea that epigenetic changes can cause type 2 diabetes. The researchers behind the new findings published in Nature Communications now aim to develop methods for disease prevention.
We inherit our genes from our parents, and they seldom change. However, epigenetic changes that arise due to environmental and lifestyle factors can affect the function of genes.
“Our new extensive study confirms our previous findings from smaller studies, showing that epigenetic changes can contribute to the development of type 2 diabetes. In this study, we have also identified new genes that impact the development of the disease. Our hope is that with the help of these results, we can develop methods that can be used to prevent type 2 diabetes,” says the study lead.
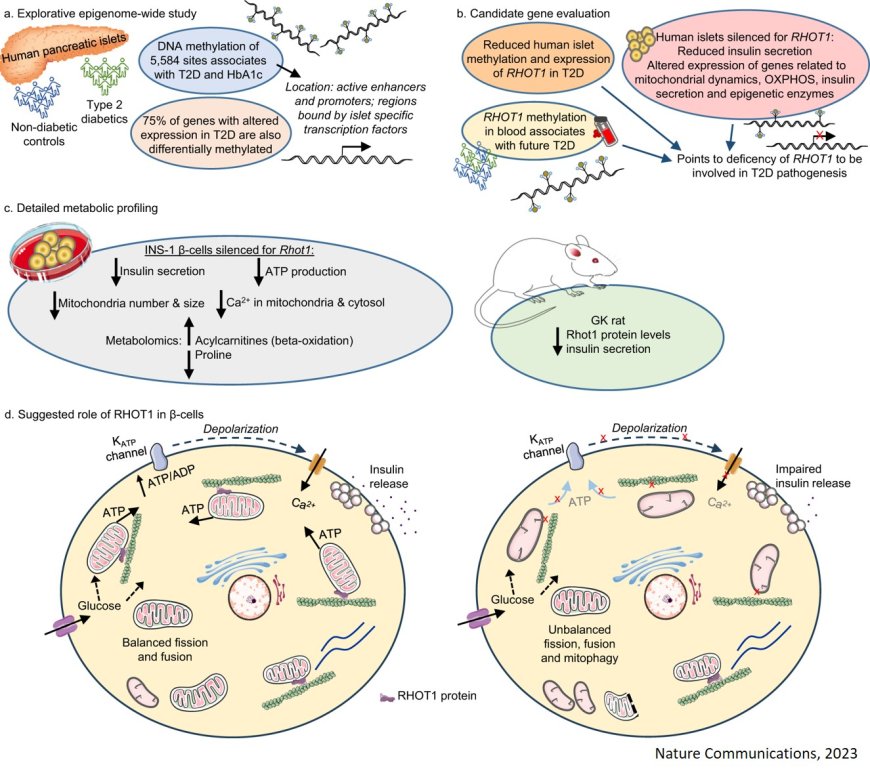
The researchers studied epigenetics in insulin-producing cells from donors and found 5584 sites in the genome with changes that differed between 25 individuals with type 2 diabetes and 75 individuals without the disease. The same epigenetic changes found in people with type 2 diabetes were also found in individuals with elevated blood sugar levels, which increase the risk of developing the disease.
“Those of us who study epigenetics, have long tried to understand whether epigenetic changes cause type 2 diabetes or if the changes occur after the disease has already developed. Because we saw the same epigenetic changes in people with type 2 diabetes and individuals at risk for the disease, we conclude that these changes may contribute to the development of type 2 diabetes," says the lead author.
The study identified 203 genes with different expression in individuals with type 2 diabetes compared to the control group. The researchers found that the gene RHOT1 showed epigenetic changes in people with type 2 diabetes and that it also played a key role in insulin secretion in insulin-producing cells. When they knocked out the gene expression of RHOT1 in cells from donors without type 2 diabetes, insulin secretion decreased.
“When we examined the same type of cells in rats with diabetes, we found a lack of RHOT1, confirming the gene’s importance for insulin secretion,” says the lead.
One goal of the research is to develop a blood-based biomarker that can predict who is at risk of developing type 2 diabetes. Therefore, the researchers investigated whether their results from insulin-producing cells in the pancreas were reflected in the blood of living people. They found epigenetic changes in the blood of a group of 540 people without the disease and they linked this to the future development of type 2 diabetes in half of the individuals.
Factors such as unhealthy diet, sedentary lifestyle, and ageing increase the risk of type 2 diabetes, and they also affect our epigenetics. With the new study, researchers have identified new mechanisms that may make it possible to develop methods to help prevent type 2 diabetes.
“If we succeed in developing an epigenetic biomarker, we can identify individuals with epigenetic changes before they become ill. These individuals can, for example, receive personalised lifestyle advice that can reduce their risk of disease, or we can develop methods that aim to correct the activity of certain genes using epigenetic editing,” says the author.