How glioblastoma tumors dodge chemotherapy
World-first research published by scientists has uncovered a mechanism that may explain why glioblastoma returns after treatment, offering new clues for future therapies.
Glioblastoma is one of the deadliest brain cancers, with a median survival rate of just 15 months. Despite surgery and chemotherapy, more than 1250 clinical trials over the past 20 years have struggled to improve survival rates.
Published in Nature Communications, the study shows that a small population of drug-tolerant cells known as “persister cells” rewires its metabolism to survive chemotherapy, using an unexpected ally as an invisibility cloak: a fertility gene called PRDM9.
“This is a world-first discovery that changes what we know about glioblastoma,” said the lead author. “By uncovering how these cancer cells recruit a fertility gene to survive treatment, we’ve opened the door to new approaches that we hope could lead to safer, more effective therapies.”
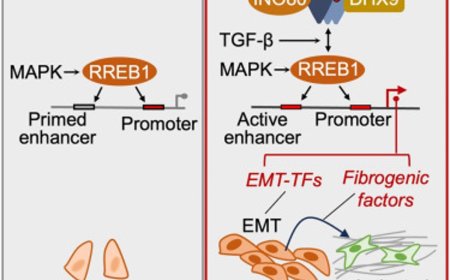
The authors identified that chemotherapy-induced PRDM9 upregulation promotes metabolic rewiring in glioblastoma stem cells, leading to chemotherapy tolerance. Mechanistically, PRDM9-dependent H3K4me3 at cholesterol biosynthesis genes enhances cholesterol biosynthesis, which persister cells rely on to maintain homeostasis under chemotherapy-induced oxidative stress and lipid peroxidation.
PRDM9 inhibition, combined with chemotherapy, results in strong anti-cancer efficacy in preclinical glioblastoma models, significantly enhancing the magnitude and duration of the antitumor response by eliminating persisters.
Previously, PRDM9 was only known as a fertility gene, active in reproductive cells at the very start of egg and sperm formation, long before fertilisation.
The researchers are now working with Australian biotech company Syntara to develop PRDM9 inhibitors for further testing in animal models, with the hope to eventually progress to human studies. The next steps are to determine whether these inhibitors can eliminate persister cells and prevent glioblastoma from returning. Trialling this in humans is likely several years away, pending successful completion of preclinical safety and efficacy studies.
“Chemotherapy kills most cancer cells, but in glioblastoma a few survive and are able to regrow the tumor. We think we’ve found their survival trick and potential ways to block it,” said the senior author.
By blocking PRDM9 or cutting off cholesterol supply, researchers were able to wipe out persister cells in lab and animal models. When combined with chemotherapy, their approach dramatically improved survival in mice.
The team also developed a new brain-penetrant chemotherapy drug, WJA88, and paired it with a cholesterol-lowering agent already tested in humans. This combination shrank tumors and extended survival in preclinical models with minimal side effects.
“PRDM9 isn’t active in most normal tissues, which makes it an incredibly selective and promising target for cancer therapy,” said the first author. “If we can eliminate the last cancer cells standing, we can stop glioblastoma from returning. That would be a game changer for patients and families.”
The researchers say this is the first time PRDM9 has been linked to cancer, potentially opening the door to safer, more targeted treatments. The team believe the same mechanism may exist in other hard to treat cancers, with plans to test the approach on ovarian cancer next.
“Cancer relapse is one of the biggest challenges in oncology. Our research shows that by directly targeting persister cells, relapse may be preventable in preclinical models,” said the author.
Experts hope the discovery could reshape cancer research and treatment globally.
“We now need to look beyond the bulk of the tumor and study rare persister cells that drive recurrence, as well as what happens after treatment ends rather than only during drug exposure,” said the author.
https://www.nature.com/articles/s41467-025-65888-5
https://sciencemission.com/PRDM9-promotes-survival-of-drug-tolerant-persister-cells