Why sepsis patients unable to fight recurring infections
Severe sepsis from bacterial or viral infections can be life-threatening and even people recovering from severe sepsis may experience long-lasting effects on the immune system, making them more susceptible to recurrent infections. The causes for this sepsis-induced immune suppression are not well understood and lack an effective treatment.
To better understand the cause, the researchers analyzed the blood stem cells of mice with prior sepsis and their results were recently published in the journal Stem Cell Reports.
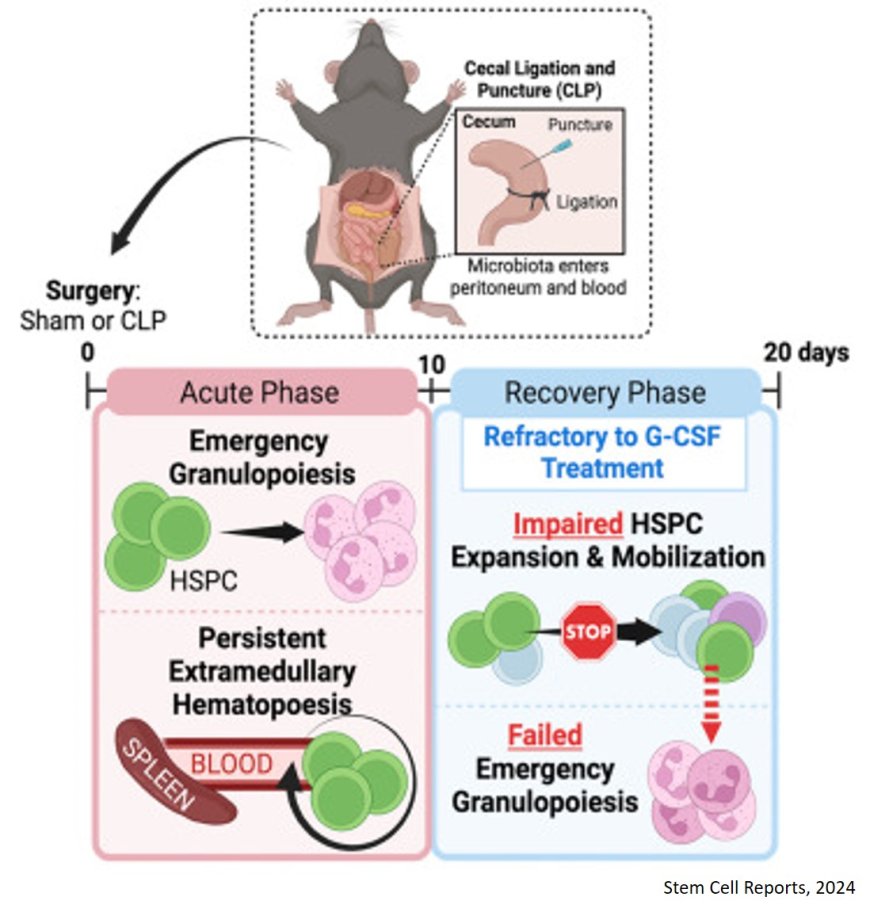
During acute infection, blood stem cells in the bone marrow are activated by signaling molecules called inflammatory cytokines, which make them divide and migrate to the blood stream to generate large quantities of immune cells outside the bone marrow. Once infection is eliminated, cytokine levels return to baseline and blood stem cell activation and immune cell production stops.
To understand how this process gets dysregulated after severe sepsis resolves, the researchers analyzed the blood stem cells of mice and found them to be fully recovered and functional in the bone marrow of mice 20 days after sepsis. However, upon a second round of inflammatory stimulation, using the stem cell mobilizing agent G-CSF, the blood stem cells of sepsis survivors did not undergo a new round of activation and mobilization as did those in mice without prior sepsis.
Consequently, immune cells were not efficiently produced in those mice with prior sepsis. These observations could explain why following sepsis, patients are unable to efficiently combat new infections and why giving inflammatory cytokines and G-CSF specifically to sepsis patients had no effect against secondary infections in previous clinical trials.
This knowledge may help to identify new treatments for patients with post-sepsis immune suppression.